Bone blockade in inflammation of the trigeminal nerve. Methods of blockade of the trigeminal nerve Where is the trigeminal nerve
Fortunately, few people are familiar with the pain that comes with neuralgia. trigeminal nerve. Many doctors consider it one of the strongest that a person can experience. The intensity of the pain syndrome is due to the fact that the trigeminal nerve provides sensitivity to most structures of the face.
Trinity - the fifth and largest pair cranial nerves. related to nerves mixed type, having motor and sensory fibers. Its name is due to the fact that the nerve is divided into three branches: ophthalmic, maxillary and mandibular. They provide sensitivity to the face, soft tissues of the cranial vault, dura mater, oral and nasal mucosa, and teeth. The motor part provides nerves (innervates) some muscles of the head.
The trigeminal nerve has two motor nuclei and two sensory nuclei. Three of them are located in the hindbrain, and one is sensitive in the middle. The motor nerves form the motor root of the entire nerve at the exit from the pons. Next to the motor fibers enter the medulla, forming a sensory root.
These roots form a nerve trunk that penetrates under the hard sheath. Near the top temporal bone fibers form a trigeminal node from which three branches emerge. The motor fibers do not enter the node, but pass under it and connect with the mandibular branch. It turns out that the ophthalmic and maxillary branches are sensory, and the mandibular branch is mixed, since it includes both sensory and motor fibers.
Branch functions
- Eye branch. Transmits information from the skin of the skull, forehead, eyelids, nose (excluding nostrils), frontal sinuses. Provides sensitivity to the conjunctiva and cornea.
- Maxillary branch. Infraorbital, pterygopalatine and zygomatic nerves, branches of the lower eyelid and lips, alveolar (posterior, anterior and middle), innervating teeth in the upper jaw.
- Mandibular branch. Medial pterygoid, ear-temporal, inferior alveolar and lingual nerves. These fibers carry information from the lower lip, teeth and gums, chin and jaw (except at a certain angle), part of the outer ear, and oral cavity. Motor fibers provide communication with chewing muscles, giving a person the opportunity to speak and eat. It should be noted that the mandibular nerve is not responsible for taste perception, it is the task of the tympanic string or the parasympathetic root of the submandibular node.
Pathologies of the trigeminal nerve are expressed in the disruption of the work of certain motor or sensory systems. Most often, trigeminal neuralgia or trigeminal neuralgia occurs - inflammation, squeezing or pinching of the fibers. In other words, it is a functional pathology of the peripheral nervous system, which is characterized by bouts of pain in half of the face.
Neuralgia of the facial nerve is predominantly an "adult" disease, it is extremely rare in children.
Attacks of neuralgia of the facial nerve are marked by pain, conditionally considered one of the strongest that a person can experience. Many patients compare it to a lightning bolt. Seizures can last from a few seconds to hours. However severe pain more characteristic of cases of inflammation of the nerve, that is, for neuritis, and not for neuralgia.

Causes of trigeminal neuralgia
The most common cause is compression of the nerve itself or a peripheral node (ganglion). Most often, the nerve is squeezed by the pathologically tortuous superior cerebellar artery: in the area where the nerve exits the brain stem, it passes close to the blood vessels. This reason often causes neuralgia with hereditary defects vascular wall and the presence of an arterial aneurysm, in combination with high blood pressure. For this reason, neuralgia often occurs in pregnant women, and after childbirth, the attacks disappear.
Another cause of neuralgia is a defect myelin sheath. The condition may develop in demyelinating diseases ( multiple sclerosis, acute disseminated encephalomyelitis, Devic optomyelitis). In this case, neuralgia is secondary, as it indicates a more severe pathology.
Sometimes compression occurs due to the development of a benign or malignant tumor nerve or meninges. So with neurofibromatosis, fibromas grow and cause various symptoms, including neuralgia.
Neuralgia can be the result of a brain injury, severe concussion, prolonged fainting. In this condition, cysts appear that can compress tissues.
Rarely, postherpetic neuralgia becomes the cause of the disease. Along the course of the nerve, characteristic blistering rashes appear, burning pains occur. These symptoms indicate damage to the nervous tissue by the herpes simplex virus.
Causes of seizures with neuralgia
When a person has neuralgia, it is not necessary that the pains are constantly noted. Attacks develop as a result of irritation of the trigeminal nerve in trigger or "trigger" zones (corners of the nose, eyes, nasolabial folds). Even with a weak impact, they generate a painful impulse.
Risk factors:
- Shaving. An experienced doctor can determine the presence of neuralgia by a thick beard in a patient.
- Stroking. Many patients refuse napkins, handkerchiefs and even makeup, protecting the face from unnecessary exposure.
- Brushing teeth, chewing food. Movement of the muscles of the oral cavity, cheeks, and constrictors of the pharynx causes displacement of the skin.
- Liquid intake. In patients with neuralgia, this process causes the most severe pain.
- Crying, laughing, smiling, talking and other actions that provoke movement in the structures of the head.
Any movement of the facial muscles and skin can cause an attack. Even a breath of wind or a transition from cold to heat can provoke pain.

Symptoms of neuralgia
Patients compare the pain in the pathology of the trigeminal nerve with a lightning discharge or a powerful electric shock that can cause loss of consciousness, tearing, numbness and dilated pupils. Pain syndrome covers one half of the face, but entirely: skin, cheeks, lips, teeth, orbits. However, the frontal branches of the nerve are rarely affected.
For this type of neuralgia, irradiation of pain is uncharacteristic. Only the face is affected, without spreading sensations to the hand, tongue or ears. It is noteworthy that neuralgia affects only one side of the face. As a rule, attacks last a few seconds, but their frequency can be different. The state of rest ("light interval") usually takes days and weeks.
Clinical picture
- Severe pain that has a piercing, penetrating or shooting character. Only one half of the face is affected.
- The skewness of certain areas or the entire half of the face. Facial expression.
- Muscle twitching.
- Hyperthermic reaction (moderate rise in temperature).
- Chills, weakness, pain in the muscles.
- Small rash in the affected area.
The main manifestation of the disease, of course, is severe pain. After the attack, facial expressions are distorted. With advanced neuralgia, changes can be permanent.
Similar symptoms can be observed with tendonitis, occipital neuralgia and Ernest's syndrome, so it is important to make a differential diagnosis. Temporal tendonitis provokes pain in the cheeks and teeth, discomfort in the neck area.
Ernest's syndrome is an injury to the stylomandibular ligament that connects the base of the skull to the mandible. The syndrome causes pain in the head, face, and neck. With neuralgia of the occipital nerve, pain is localized in the back of the head and passes into the face.
The nature of the pain
- Typical. Shooting sensations, reminiscent of electric shocks. As a rule, they occur in response to touching certain areas. Typical pain is manifested by seizures.
- Atypical. Constant pain that captures most of the face. There are no fading periods. Atypical pain in neuralgia is more difficult to cure.
Neuralgia is a cyclic disease: periods of exacerbation alternate with remission. Depending on the degree and nature of the lesion, these periods have different durations. Some patients experience pain once a day, others complain of attacks every hour. However, in all pain begins abruptly, reaching a peak in 20-25 seconds.

Toothache
The trigeminal nerve consists of three branches, two of which provide sensation to the oral region, including the teeth. All unpleasant sensations are transmitted by the branches of the trigeminal nerve to their half of the face: a reaction to cold and hot, pains of a different nature. It is not uncommon for people with trigeminal neuralgia to go to the dentist, mistaking the pain for a toothache. However, rare patients with pathologies dental system come to the neurologist with suspicions of neuralgia.
How to distinguish toothache from neuralgia:
- When a nerve is damaged, the pain is similar to an electric shock. Attacks are mostly short, and the intervals between them are long. There is no discomfort in between.
- Toothache usually does not start and end suddenly.
- The strength of pain in neuralgia makes a person freeze, pupils dilate.
- Toothache can begin at any time of the day, and neuralgia manifests itself exclusively during the day.
- Analgesics help relieve toothache, but they are practically ineffective for neuralgia.
Distinguishing a toothache from inflammation or a pinched nerve is simple. Toothache most often has a wave-like course, the patient is able to point to the source of the impulse. There is an increase in discomfort during chewing. The doctor can take a panoramic x-ray of the jaw, which will reveal the pathology of the teeth.
Odontogenic (tooth) pain occurs many times more often than manifestations of neuralgia. This is due to the fact that pathologies of the dentoalveolar system are more common.
Diagnostics
With severe symptoms, the diagnosis is not difficult. The main task of the doctor is to find the source of neuralgia. Differential Diagnosis should be aimed at excluding oncology or another cause of compression. In this case, one speaks of a true condition, not a symptomatic one.
Examination methods:
- High-resolution MRI (magnetic field strength greater than 1.5 Tesla);
- computed angiography with contrast.

Conservative treatment of neuralgia
Possibly conservative and surgery trigeminal nerve. Almost always, conservative treatment is used first, and if it is ineffective, surgery is prescribed. Patients with such a diagnosis are put on sick leave.
Drugs for treatment:
- Anticonvulsants (anticonvulsants). They are able to eliminate congestive excitation in neurons, which is similar to a convulsive discharge in the cerebral cortex in epilepsy. For these purposes, drugs with carbamazepine (Tegretol, Finlepsin) are prescribed at 200 mg per day with a dose increase to 1200 mg.
- Muscle relaxants of central action. These are Mydocalm, Baclofen, Sirdalud, which allow you to eliminate muscle tension and spasms in neurons. Muscle relaxants relax the "trigger" zones.
- Analgesics for neuropathic pain. They are used if there are burning pains caused by a herpes infection.
Physiotherapy for trigeminal neuralgia can relieve pain by increasing tissue nutrition and blood supply in the affected area. Thanks to this, it happens accelerated recovery nerve.
Physiotherapy for neuralgia:
- UHF (Ultra High Frequency Therapy) improves microcirculation to prevent masticatory muscle atrophy;
- UVR (ultraviolet radiation) helps relieve pain from nerve damage;
- electrophoresis with novocaine, diphenhydramine or platifillin relaxes muscles, and the use of B vitamins improves the nutrition of the myelin sheath of nerves;
- laser therapy stops the passage of an impulse through the fibers, stopping pain;
- electric currents (impulsive mode) can increase remission.
It should be remembered that antibiotics are not prescribed for neuralgia, and taking conventional painkillers does not give a significant effect. If conservative treatment does not help and the intervals between attacks are reduced, surgical intervention is required.
Massage for neuralgia of the face
Massage for neuralgia helps eliminate muscle tension and increase tone in atonic (weakened) muscles. Thus, it is possible to improve microcirculation and blood supply in the affected tissues and directly in the nerve.
Massage involves the impact on the exit zones of the nerve branches. This is the face, ears and neck, then the skin and muscles. Massage should be carried out in a sitting position, with your head back on the headrest and allowing the muscles to relax.
Start with light massaging movements. It is necessary to focus on the sternocleidomastoid muscle (on the sides of the neck), then move up to the parotid regions. Here the movements should be stroking and rubbing.
The face should be massaged gently, first the healthy side, then the affected one. The duration of the massage is 15 minutes. The optimal number of sessions per course is 10-14.

Surgery
As a rule, patients with trigeminal nerve pathology are offered surgery after 3-4 months of unsuccessful conservative treatment. Surgical intervention may imply the elimination of the cause or a decrease in the conduction of impulses along the branches of the nerve.
Operations that eliminate the cause of neuralgia:
- removal of neoplasms from the brain;
- microvascular decompression (removal or displacement of vessels that have expanded and put pressure on the nerve);
- expansion of the exit of the nerve from the skull (the operation is performed on the bones of the infraorbital canal without aggressive intervention).
Operations to reduce the conduction of pain impulses:
- radiofrequency destruction (destruction of altered nerve roots);
- rhizotomy (dissection of fibers using electrocoagulation);
- balloon compression (compression of the trigeminal ganglion with subsequent death of the fibers).
The choice of method will depend on many factors, but if the operation is chosen correctly, the attacks of neuralgia stop. The physician must take into account general state patient, the presence of concomitant pathologies, the causes of the disease.
Surgical techniques
- Blockade of individual sections of the nerve. A similar procedure is prescribed in the presence of severe comorbidities in old age. The blockade is carried out with the help of novocaine or alcohol, providing an effect for about a year.
- ganglion blockade. The doctor gains access to the base of the temporal bone, where the Gasser node is located, through a puncture. Glycerol is injected into the ganglion (glycerol percutaneous rhizotomy).
- Transection of the trigeminal nerve root. This is a traumatic method, which is considered radical in the treatment of neuralgia. For its implementation, extensive access to the cranial cavity is needed, therefore, trepanation is performed and burr holes are applied. At the moment, the operation is carried out extremely rarely.
- Dissection of the bundles that lead to the sensitive nucleus in medulla oblongata. The operation is performed if the pain is localized in the projection of the Zelder zones or distributed according to the nuclear type.
- Decompression of the Gasser's node (Operation Janette). The operation is prescribed for squeezing the nerve with a vessel. The doctor separates the vessel and the ganglion, isolating it with a muscle flap or a synthetic sponge. Such an intervention relieves the patient of pain for a short period of time, without depriving him of sensitivity and without destroying the nervous structures.
It must be remembered that most operations for neuralgia deprive the affected side of the face of sensitivity. This causes inconvenience in the future: you can bite your cheek, not feel pain from injury or damage to the tooth. Patients who have undergone such an intervention are advised to visit the dentist regularly.

Gamma Knife and Particle Accelerator in Healing
Modern medicine offers patients with trigeminal neuralgia minimally invasive and therefore atraumatic neurosurgical operations. They are carried out using a particle accelerator and a gamma knife. They are relatively recently known in the CIS countries, and therefore the cost of such treatment is quite high.
The doctor directs beams of accelerated particles from ring sources into a specific area of the brain. The cobalt-60 isotope emits a beam of accelerated particles that burns out the pathogenic structure. The processing accuracy reaches 0.5 mm, and the rehabilitation period is minimal. The patient can go home immediately after the operation.
Folk ways
There is an opinion that it is possible to relieve pain in trigeminal neuralgia with the help of black radish juice. The same remedy is effective for sciatica and intercostal neuralgia. It is necessary to moisten a cotton pad with juice and gently rub it into the affected areas along the nerve.
Another effective remedy – fir oil. It not only relieves pain, but also helps to restore the nerve with neuralgia. It is necessary to moisten a cotton swab with oil and rub along the length of the nerve. Since the oil is concentrated, you should not work hard, otherwise you may burn. You can repeat the procedure 6 times a day. The course of treatment is three days.
Fresh geranium leaves are applied to the affected areas with neuralgia for several hours. Repeat twice a day.
The treatment regimen for a stiff trigeminal nerve:
- Warming up your feet before bed.
- Taking vitamin B tablets and a teaspoon of flower bee bread twice a day.
- Twice a day, smear the affected areas with the Vietnamese "Asterisk".
- Drink hot tea with soothing herbs at night (motherwort, lemon balm, chamomile).
- Sleep in a hat with rabbit fur.
When the pain affects the teeth and gums, chamomile infusion can be used. In a glass of boiling water, insist a teaspoon of chamomile for 10 minutes, then filter. It is necessary to take the tincture in your mouth and rinse until it cools. You can repeat the procedure several times a day.
Tinctures
- Hop cones. Pour raw materials with vodka (1: 4), leave for 14 days, shake daily. Drink 10 drops twice a day after meals. Must be diluted with water. To normalize sleep and calm the nervous system, you can stuff a pillow with hop cones.
- Garlic oil. This tool can be bought at a pharmacy. In order not to lose essential oils, need to do alcohol tincture: add a teaspoon of oil to a glass of vodka and rub the whiskey with the resulting mixture twice a day. Continue the course of treatment until the seizures disappear.
- Althea root. To prepare the medicine, you need to add 4 teaspoons of raw materials to a glass of cooled boiled water. The agent is left for a day, in the evening gauze is moistened in it and applied to the affected areas. From above the gauze is covered with cellophane and a warm scarf. It is necessary to keep the compress for 1-2 hours, then wrap your face with a scarf for the night. Usually the pain stops after a week of treatment.
- Duckweed. This remedy is suitable for removing puffiness. To prepare duckweed tincture, you need to prepare it in the summer. Add a spoonful of raw materials to a glass of vodka, leave for a week in a dark place. The medium is filtered several times. Take 20 drops mixed with 50 ml of water three times a day until complete recovery.

Blockade of the first branch of the trigeminal nerve
The first branch of the trigeminal nerve - n. ophtalmicus is divided into three branches:
- n. frontalis,
- n. lacrymalis,
- n. nasociliaris.
The blockade of these individual branches, according to the methods described by Brown and Peakert, consists in injecting local anesthetic, in particular novocaine, into the orbit according to the course of these nerves, outside of the muscle cover eyeball- bulbus oculi.
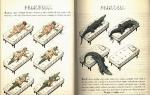
Damage to the eyeball is easy to avoid if you follow the proposed rules. For this, straight long needles are used; the use of curved varieties, as recommended by some, is not necessary, and Brown warned against this as early as the beginning of the 20th century. Injection into individual nerve endings of the first branch of the trigeminal nerve is performed exactly in those places where, according to the anatomical structure of the bony cavity of the orbit, there are the best and most reliable ways for passing the needle. The point of the latter must penetrate into the orbit when guiding over the bone, and this is only possible where the bony wall of the orbit is flatter and not too concave. Such places are located on the lateral and on the upper part. medial wall orbits; on its lower wall there is also a mostly flat bone surface, so that a blockade can also be carried out here. The photo below shows the inserted needles for medial and lateral orbital injections.
Medial injection anesthetizes the branches of n. nasociliaris and nn. ethmoidales; lateral injection - n. frontalis and n. lacrymalis.
The injection points for these three orbital injections are shown in the photo below.

Blockade of the first branch of the trigeminal nerve through lateral injection of the orbit
At the point "a", lying above the most lateral corner of the eye, a lateral injection is made, for anesthesia n. frontalis and n. lacrymalis.
According to Brown, a needle is injected at this point so that its tip, hitting the bone, does not leave the bone anymore, and then the needle is inserted to a depth of 4½-5 cm to the fissura orbitalis super. Here they run into the upper wall of the orbit, so that further advancement of the tip is impossible. Brown here injects 5 ml of a 1% solution of novocaine with adrenaline into the circumference of fissura orbitalis superior; Hartel advises to penetrate to a maximum depth of 3 cm and only then inject a local anesthetic.
With this lateral injection of the orbit, anesthesia of the skin occurs at the lateral angle of the eye, at the medial angle of the eye, on the upper eyelid, on the forehead and crown; in addition, there is anesthesia of the conjunctiva of the lateral and medial parts upper eyelid and parts of the conjunctiva of the lower eyelid.
Blockade of the first branch of the trigeminal nerve through the medial injection of the orbit
With a medial injection of the orbit, for anesthesia nn. ethmoidales the point of injection will be point "b". It lies, according to Brown, a finger above the inner corner of the eye (see photo above).
The needle is inserted here, under the control of palpation with the tip of the bone, to a depth of 4-5 cm in the horizontal direction. Brown injects here 5 ml of a 1% solution of novocaine with adrenaline, calculated on the medial and upper wall of the orbit.
According to Hartel for blockade n. ethmoidalis ant., which innervates the upper and anterior part of the nasal mucosa and the skin of the tip of the nose, the needle should be inserted about 2 cm deep. This depth is not enough to reach n. ethmoidalis post., which supplies the posterior cells of the ethmoid bone and the cavity of the sphenoid. Since with a deeper injection in the direction of the foramen ethmoidale post, they get too close to the optic nerve, Hartel suggests making a medial injection of the orbit, no deeper than 3 cm, counting on the diffusion of the solution to a greater depth.
After injection into the orbit, Brown's experience shows a rapidly passing protrusio bulbi with swelling of the upper eyelid. There are no complications. Since the injection of the orbit is carried out according to Brown along the bone wall outside the circulus tendineus and the muscle funnel of the bulbus oculi, the influence on n. opticus and on nn. ciliares was not observed. According to Kredel, in connection with the injection of the orbit, the appearance of amaurosis was noted, lasting about ten minutes. It could have been caused by adrenaline or by the local anesthetic itself. Voyno-Yasenetsky observed passing amaurosis, which occurred only a day after the operation and was caused by inflammatory edema of the orbit. This case must be considered as a consequence of local anesthesia for frontal sinus empyema.
Retrobulbar blockade
For anesthesia of the eyeball during enucleation or exenteration, it is necessary to produce a retrobulbar blockade of nn. ciliares and ggl. ciliare.
Lowenstein for this purpose injected a needle at the middle of the lateral edge of the orbit, to a depth of 4½ cm into the orbit, between the eyeball and the conjunctiva; here he turned the needle to the medial side, approached n. opticus and ganglion ciliare. He injected here 1 ml of a 1% solution of cocaine with adrenaline. Next, he injected ½ ml of the same solution around the eyeball.
Siegrist injected with curved needles retrobulbar tissue in a circle, from four conjunctival injection points.
Mende for retrobulbar blockade recommended inserting a needle behind the eyeball from two injection points, temporal and nasal, near the entry point optic nerve and nn. ciliares; he injected about 2 ml of a 1 or 2% solution of novocaine with adrenaline. In addition, 1 ml of the same solution was injected subconjunctivally near the site of attachment of the rectus muscle.
Seidel injected 1-2 ml of a 1% solution of novocaine with adrenaline subconjunctivally, around the eyeball. Then he injected from four points 1 ml of the solution retrobulbar through the conjunctiva and 1 ml of the same solution during the penetration of the needle into the retrobulbar tissue.
Blockade of the second branch of the trigeminal nerve
The second branch of the trigeminal nerve - n. maxillaris, as it passes through the foramen rotundum at the base of the skull, can be reached with an injection needle in various ways. This nerve trunk runs horizontally from the foramen rotundum into the pterygopalatine fossa, which it passes towards the canalis infraorbitalis. Having passed this channel, it appears as n. infraorbitalis from the opening of the same name.
One can now get into the second branch of the trigeminal nerve at the foramen rotundum or in the intraorbital route, or as tried before, by inserting the needle under the zygomatic arch and advancing it along the posterior surface of the maxilla into the fossa pterygopalatina.
The orbital pathway, according to Hartel, was first proposed by Payer, but implemented and methodically developed first. Hartel calls this path "axial puncture foramen rotundum".
If on the skull, on the lateral part of the lower edge of the orbit, the needle is passed straight inward, then they enter through the fissura inferior into the canalis infraorbitalis, between the sphenoid bone and the upper jaw; at the end of this channel lies the foramen rotundum. First, the needle encounters some obstruction at the planum pterygoideum of the sphenoid bone.
If we now lead the needle along this obstacle and in the middle, then the foramen rotundum is reached.
The distance of the foramen rotundum from the lower edge of the orbit is approximately 4-5 cm.
Since the foramen rotundum is very narrow and completely filled with n. maxillaris, the needle is strongly opposed and the injection requires sufficient pressure. If you get into the nerve, then the patient feels pain diverging along the area of \u200b\u200binnervation of the second branch of the trigeminal nerve.
Intraorbital blockade of the second branch of the trigeminal nerve according to Hartel
 Orbital blockade of the second branch of the trigeminal nerve in the foramen rotundum
Orbital blockade of the second branch of the trigeminal nerve in the foramen rotundum
According to Hartel, the technique of intraorbital blockade n. maxillaris in the foramen rotundum is as follows:
The needle is inserted at the lower edge of the orbit, in the middle between the sutura zygomaticomaxillaris and the outer lower edge of the orbit. With the index finger of the left hand, the eyeball is pushed upward and the needle is passed between the finger and the lower wall of the orbit sagittally and horizontally inward until, after passing through the fissura orbitalis inferior, it stumbles at a depth of 4-5 cm on the planum pterigoideum of the sphenoid bone. From this bone obstacle, a passage is palpated in depth in the direction and inward until complaints of pain radiating to area n appear. maxillaris. Having hit the foramen rotundum with a needle, it is carried out into it for a few more millimeters and injected at a certain pressure with ½ ml of a 2% solution of novocaine with adrenaline. With a successful injection, anesthesia of the entire area innervated by the second branch of the trigeminal nerve occurs immediately.
The direction of the inserted needle is shown in the photo above with an arrow.
Blockade of the second branch of the trigeminal nerve according to Brown
 Blockade of the second branch of the trigeminal nerve in the foramen rotundum with an injection under the zygomatic arch
Blockade of the second branch of the trigeminal nerve in the foramen rotundum with an injection under the zygomatic arch
Blockade n. maxillaris in the fossa pterygopalatina from an injection point under the zygomatic arch was first performed by Matas in 1900. Schlosser used this method to alcoholize the trigeminal nerve in neuralgia, and Braun used this technique for local anesthesia.
According to Hartel, only in 33% of cases it is possible to penetrate this way with the tip of the needle into the foramen rotundum, in most cases the action of the blockade is explained by the penetration of the local anesthetic to the nerve through diffusion in the loose fatty tissue of the fossa pterygopalatina.
According to Brown, the blockade technique n. maxillaris from the lower edge of the zygomatic arch is as follows:
The needle is inserted under the lower angle of the zygomatic bone and moves inward and upward. It slides along the tuber maxillare and if it is too curved, then the injection point should be chosen more posteriorly. Sometimes the needle clings to the large wing of the sphenoid bone; then you need to carefully change direction. At a depth of 5-6 cm, they fall into the fossa on the nerve.
Brown injected 5 ml of a 1% solution of novocaine with adrenaline into this place with a slight advance and pulling of the needle. While pulling, he injected another 5 ml of the same solution behind the upper jaw to cause contraction of the branches of art. maxillaris. If you hit n correctly. maxillaris, the patient again feels widespread pain in the face. If the advancement of the needle along the tuber maxillare is difficult, then under some circumstances it is necessary to make a new injection, more under the middle of the zygomatic bone and drive a double dose of a solution of novocaine with adrenaline, that is, 10 ml of a 1% solution, so that the anesthetic can reach the nerve by diffusion.
In the photo above, the needle was inserted into the foramen rotundum from under the zygomatic arch; the arrow shows the direction.
Ostwalf maxillary nerve block
It should also be mentioned about the method of anesthesia n. maxillaris according to Ostwalf, who injects the needle from the side of the oral cavity behind the last molar and advances it forward along the planum infratemporale, entering the fossa pterygoidea.
Maxillary nerve block by Offerhaus
The next method of anesthesia of the maxillary nerve is according to Offerhaus. He measures the distance between the middles of both zygomatic arches with a compass and, subtracting from the measurement obtained the distance between the upper alveolar processes behind the molars, determines how far the foramen rotundum is from its point of injection. The latter is located either above or below the middle of the zygomatic bone.
Blockade of the third branch of the trigeminal nerve
The third branch of the trigeminal nerve, the region of sensitive innervation of which has already been discussed in one of the articles on our website, goes to the base of the skull through the foramen ovale.
Ostwalt mandibular nerve block
Ostwalt, to make alcoholization of the trigeminal nerve, introduced an angled needle with the mouth open behind the third upper molar through m. pterygoideus and reached the foramen ovale.
Blockade of the mandibular nerve according to Schltisser
Schltisser uses, also for the purpose of alcoholization of the third branch n. trigeminus, another way. He inserts the needle at the front edge m. masseter, pierces the cheek and reaches the oral cavity. Here he gropes for the needle with a finger inserted into the mouth, and pushes it further, to the greater wing of the sphenoid bone. The point should now be a few millimeters from the foramen ovale. This method is so bad that if the blockade is performed incorrectly, the mucous membrane of the mouth can be pierced.
Brown mandibular nerve block
Harris, Alexander, Offerhaus and Braun take the transverse path to reach the foramen ovale.
According to Brown, the injection point lies under the middle of the zygomatic bone. The needle is advanced obliquely into the skull. And here it is best to have a model of the skull near you, on which the oblique direction is fixed with another needle.
The structure of the trigeminal nerve
The trigeminal nerve is the fifth and largest pair of cranial nerves. Refers to the nerves of the mixed type, having motor and sensory fibers. Its name is due to the fact that the nerve is divided into three branches: ophthalmic, maxillary and mandibular. They provide sensitivity to the face, soft tissues of the cranial vault, dura mater, oral and nasal mucosa, and teeth. The motor part provides nerves (innervates) some muscles of the head.
The trigeminal nerve has two motor nuclei and two sensory nuclei. Three of them are located in the hindbrain, and one is sensitive in the middle. The motor nerves form the motor root of the entire nerve at the exit from the pons. Near the motor root, sensory fibers enter the medulla to form the sensory root.
These roots form the trunk of the trigeminal nerve, penetrating under the hard shell. Near the apex of the temporal bone, the fibers form the trigeminal ganglion, from which three branches of the nerve emerge. The motor fibers do not enter the node, but pass under it and connect with the mandibular branch. It turns out that the ophthalmic and maxillary branches are sensory, and the mandibular mixed, since it includes both sensory and motor fibers.
Functions of the branches of the trigeminal nerve
- Eye branch. Transmits information from the skin of the skull, forehead, eyelids, nose (excluding nostrils), frontal sinuses. Provides sensitivity to the conjunctiva and cornea.
- Maxillary branch. Infraorbital, pterygopalatine and zygomatic nerves, branches of the lower eyelid and lower lip, alveolar branches (posterior, anterior and middle), innervating the teeth in the upper jaw.
- Mandibular branch. Medial pterygoid, ear-temporal, inferior alveolar and lingual nerves. These fibers transmit information from the lower lip, teeth and gums, chin and jaw (except at a certain angle), part of the outer ear and oral cavity. Motor fibers provide communication with the masticatory muscles, giving a person the ability to speak and chew. It should be noted that the mandibular nerve is not responsible for taste perception, it is the task of the tympanic string or the parasympathetic root of the submandibular node, which enters the lingual nerve.
Pathologies of the trigeminal nerve are expressed in the disruption of the work of certain motor or sensory systems. The most common is trigeminal neuralgia or trigeminal neuralgia - inflammation, squeezing or pinching of the fibers. In other words, it is a functional pathology of the peripheral nervous system, which is characterized by bouts of pain in half of the face.
Neuralgia of the facial nerve is predominantly an "adult" disease, it is extremely rare in children.
Attacks of neuralgia of the facial nerve are marked by pain, conditionally considered one of the strongest that a person can experience. Many patients compare it to a lightning bolt. Seizures can last from a few seconds to hours. However, severe pain is more characteristic of cases of inflammation of the nerve, that is, for neuritis, and not for neuralgia.

Causes of trigeminal neuralgia
The most common cause of trigeminal neuralgia is compression of its own or peripheral node (ganglion). Most often, the nerve is squeezed by the pathologically tortuous superior cerebellar artery: in the area where the nerve exits the brain stem, it passes close to the blood vessels. This cause often causes neuralgia with hereditary defects in the vascular wall and the presence of an arterial aneurysm, in combination with high blood pressure. For this reason, neuralgia often occurs in pregnant women, and after childbirth, the attacks disappear.
Another cause of trigeminal neuralgia is a defect in the myelin sheath. The condition can develop in demyelinating diseases (multiple sclerosis, acute disseminated encephalomyelitis, Devic optomyelitis). In this case, neuralgia is secondary, as it indicates a more severe pathology.
Sometimes compression occurs due to the development of a benign or malignant tumor of the nerve or meninges. So with neurofibromatosis, fibromas grow and cause various symptoms, including neuralgia.
Trigeminal neuralgia can be the result of a brain injury, severe concussion, prolonged fainting. In this condition, cysts appear that can compress tissues.
Rarely, postherpetic neuralgia becomes the cause of the disease. Along the course of the nerve, characteristic blistering rashes appear, burning pains occur. These symptoms indicate damage to the nervous tissue by the herpes simplex virus.
Causes of seizures with neuralgia
When a person has neuralgia, it is not necessary that the pains are constantly noted. Attacks develop as a result of irritation of the trigeminal nerve in trigger or "trigger" zones (corners of the nose, eyes, nasolabial folds). Even with a weak impact, they generate a painful impulse.
Risk factors:
- Shaving. An experienced doctor can determine the presence of neuralgia by a thick beard in a patient.
- Stroking. Many patients refuse napkins, handkerchiefs and even makeup, protecting the face from unnecessary exposure.
- Brushing teeth, chewing food. Movement of the muscles of the oral cavity, cheeks, and constrictors of the pharynx causes displacement of the skin.
- Liquid intake. In patients with trigeminal neuralgia, this process causes the most severe pain.
- Crying, laughing, smiling, talking and other actions that provoke movement in the structures of the head.
Any movement of the facial muscles and skin can cause an attack. Even a breath of wind or a transition from cold to heat can provoke pain.

Symptoms of trigeminal neuralgia
Patients compare the pain of trigeminal neuralgia to a lightning bolt or a powerful electric shock that can cause loss of consciousness, tearing, numbness, and dilated pupils. Pain syndrome covers one half of the face, but entirely: skin, cheeks, lips, teeth, orbits. However, the frontal branches of the nerve are rarely affected.
For this type of neuralgia, irradiation of pain is uncharacteristic. Only the face is affected, without spreading sensations to the hand, tongue or ears. It is noteworthy that neuralgia affects only one side of the face. As a rule, attacks last a few seconds, but their frequency can be different. The state of rest ("light interval") usually takes days and weeks.
Clinical picture of trigeminal neuralgia
- Severe pain that has a piercing, penetrating or shooting character. Only one half of the face is affected.
- The skewness of certain areas or the entire half of the face. Facial expression.
- Muscle twitching.
- Hyperthermic reaction (moderate rise in temperature).
- Chills, weakness, pain in the muscles.
- Small rash in the affected area.
The main manifestation of trigeminal neuralgia, of course, is severe pain. After the attack, facial expressions are distorted. With advanced neuralgia, changes can be permanent.
Similar symptoms can be observed with tendonitis, occipital neuralgia and Ernest's syndrome, so it is important to make a differential diagnosis. Temporal tendinitis provokes pain in the cheeks and teeth, there is a headache and discomfort in the neck.
Ernest's syndrome is an injury to the stylomandibular ligament that connects the base of the skull to the mandible. The syndrome causes pain in the head, face, and neck. With neuralgia of the occipital nerve, pain is localized in the back of the head and passes into the face.
The nature of pain in trigeminal neuralgia
- Typical. Shooting sensations, reminiscent of electric shocks. As a rule, they occur in response to touching certain areas. Typical pain is manifested by seizures.
- Atypical. Constant pain that captures most of the face. There are no quiet periods. Atypical pain in neuralgia is more difficult to cure.
Trigeminal neuralgia is a cyclic disease: periods of exacerbation alternate with periods of remission. Depending on the degree and nature of the lesion, these periods have different durations. Some patients experience pain once a day, others complain of attacks every hour. However, in all pain begins abruptly, reaching a peak in 20-25 seconds.

Toothache with trigeminal neuralgia
The trigeminal nerve consists of three branches, two of which provide sensation to the oral region, including the teeth. All unpleasant sensations are transmitted by the branches of the trigeminal nerve to their half of the face: a reaction to cold and hot, pains of a different nature. It is not uncommon for people with trigeminal neuralgia to go to the dentist, mistaking the pain for a toothache. However, rarely patients with pathologies of the dentoalveolar system come to the neurologist with suspicions of neuralgia.
How to distinguish a toothache from trigeminal neuralgia:
- When a nerve is damaged, the pain is similar to an electric shock. Attacks are mostly short, and the intervals between them are long. There is no discomfort in between.
- Toothache usually does not start and end suddenly.
- The strength of pain in neuralgia makes a person freeze, pupils dilate.
- Toothache can begin at any time of the day, and neuralgia manifests itself exclusively during the day.
- Analgesics help relieve toothache, but they are practically ineffective for neuralgia.
Distinguishing a toothache from inflammation or a pinched nerve is simple. Toothache most often has a wave-like course, the patient is able to point to the source of the impulse. There is an increase in discomfort during chewing. The doctor can take a panoramic x-ray of the jaw, which will reveal the pathology of the teeth.
Odontogenic (tooth) pain occurs many times more often than manifestations of trigeminal neuralgia. This is due to the fact that pathologies of the dentoalveolar system are more common.
Diagnosis of trigeminal neuralgia
With severe symptoms, the diagnosis is not difficult. The main task of the doctor is to find the source of neuralgia. Differential diagnosis should be aimed at excluding oncology or another cause of compression. In this case, one speaks of a true condition, not a symptomatic one.
Methods of examination for trigeminal neuralgia:
- High-resolution MRI (magnetic field strength greater than 1.5 Tesla);
- computed angiography with contrast.

Conservative treatment of neuralgia
Perhaps conservative and surgical treatment of trigeminal neuralgia. Almost always, conservative treatment is used first, and if it is ineffective, surgery is prescribed. Patients with such a diagnosis are put on sick leave.
Drugs for the treatment of trigeminal neuralgia:
- Anticonvulsants (anticonvulsants). They are able to eliminate congestive excitation in neurons, which is similar to a convulsive discharge in the cerebral cortex in epilepsy. For these purposes, drugs with carbamazepine (Tegretol, Finlepsin) are prescribed at 200 mg per day with a dose increase to 1200 mg.
- Muscle relaxants of central action. These are Mydocalm, Baclofen, Sirdalud, which allow you to eliminate muscle tension and spasms in the neurons responsible for muscle tone. Muscle relaxants relax the "trigger" zones.
- Analgesics for neuropathic pain. They are used if there are burning pains caused by a herpes infection.
Physiotherapy for trigeminal neuralgia can relieve pain by increasing tissue nutrition and blood supply in the affected area. Due to this, accelerated nerve recovery occurs.
Physiotherapy for neuralgia:
- UHF (Ultra High Frequency Therapy) improves microcirculation to prevent masticatory muscle atrophy;
- UVR (ultraviolet radiation) helps relieve pain from nerve damage;
- electrophoresis with novocaine, diphenhydramine or platifillin relaxes muscles, and the use of B vitamins improves the nutrition of the myelin sheath of nerves;
- laser therapy stops the passage of an impulse through the fibers, stopping pain;
- electric currents (impulsive mode) can increase remission.
It should be remembered that antibiotics are not prescribed for trigeminal neuralgia, and taking conventional painkillers does not give a significant effect. If conservative treatment does not help and the intervals between attacks are reduced, surgical intervention is required.
Massage for neuralgia of the face
Massage for trigeminal neuralgia helps eliminate muscle tension and increase tone in atonic (weakened) muscles. Thus, it is possible to improve microcirculation and blood supply in the affected tissues and directly in the nerve.
Massage involves the impact on the exit zones of the nerve branches. This is the face, ears and neck, then the skin and muscles. Massage should be carried out in a sitting position, with your head back on the headrest and allowing the muscles to relax.
Start with light massaging movements. It is necessary to focus on the sternocleidomastoid muscle (on the sides of the neck), then go to the parotid regions. Here the movements should be stroking and rubbing.
The face should be massaged gently, first the healthy side, then the affected one. The duration of the massage is 15 minutes. The optimal number of sessions per course is 10-14.

Surgical treatment of facial neuralgia
As a rule, patients with trigeminal neuralgia are offered surgery after 3-4 months of unsuccessful conservative treatment. Surgical intervention may involve removing the cause or reducing the conduction of impulses along the branches of the nerve.
Operations that eliminate the cause of neuralgia:
- removal of neoplasms from the brain;
- microvascular decompression (removal or displacement of vessels that have expanded and put pressure on the nerve);
- expansion of the exit of the nerve from the skull (the operation is performed on the bones of the infraorbital canal without aggressive intervention in the skull).
Operations to reduce the conduction of pain impulses:
- radiofrequency destruction (destruction of altered nerve roots);
- rhizotomy (dissection of fibers using electrocoagulation);
- balloon compression (compression of the trigeminal ganglion with subsequent death of the fibers).
The choice of method will depend on many factors, but if the operation is chosen correctly, the attacks of trigeminal neuralgia stop. The doctor must take into account the general condition of the patient, the presence of concomitant pathologies, the causes of the disease.
Surgical techniques for the treatment of neuralgia
- Blockade of individual sections of the nerve. A similar procedure is prescribed in the presence of severe comorbidities in old age. The blockade is carried out with the help of novocaine or alcohol, providing an effect for about a year.
- ganglion blockade. The doctor gains access to the base of the temporal bone, where the Gasser node is located, through a puncture. Glycerol is injected into the ganglion (glycerol percutaneous rhizotomy).
- Transection of the trigeminal nerve root. This is a traumatic method, which is considered radical in the treatment of neuralgia. For its implementation, extensive access to the cranial cavity is needed, therefore, trepanation is performed and burr holes are applied. At the moment, the operation is carried out extremely rarely.
- Dissection of the bundles that lead to the sensory nucleus in the medulla oblongata. The operation is performed if the pain is localized in the projection of the Zelder zones or distributed according to the nuclear type.
- Decompression of the Gasser's node (Operation Janette). The operation is prescribed for squeezing the nerve with a vessel. The doctor separates the vessel and the ganglion, isolating the vessel with a muscle flap or a synthetic sponge. Such an intervention relieves the patient of pain for a short period of time, without depriving him of sensitivity and without destroying the nervous structures.
It must be remembered that most operations for trigeminal neuralgia deprive the affected side of the face of sensitivity. This causes inconvenience in the future: you can bite your cheek, not feel pain from injury or damage to the tooth. Patients who have undergone such an intervention are advised to visit the dentist regularly.

Gamma knife and particle accelerator in the treatment of neuralgia
Modern medicine offers patients with trigeminal neuralgia minimally invasive and therefore atraumatic neurosurgical operations. They are carried out using a particle accelerator and a gamma knife. They are relatively recently known in the CIS countries, and therefore the cost of such treatment is quite high.
The doctor directs beams of accelerated particles from ring sources into a specific area of the brain. The cobalt-60 isotope emits a beam of accelerated particles that burns out the pathogenic structure. The processing accuracy reaches 0.5 mm, and the rehabilitation period is minimal. The patient can go home immediately after the operation.
Folk methods of treatment of neuralgia of the face
There is an opinion that it is possible to relieve pain in trigeminal neuralgia with the help of black radish juice. The same remedy is effective for sciatica and intercostal neuralgia. It is necessary to moisten a cotton pad with juice and gently rub it into the affected areas along the nerve.
Another effective remedy is fir oil. It not only relieves pain, but also helps to restore the nerve with neuralgia. It is necessary to moisten a cotton swab with oil and rub along the length of the nerve. Since the oil is concentrated, you should not work hard, otherwise you may burn. You can repeat the procedure 6 times a day. The course of treatment is three days.
Fresh geranium leaves are applied to the affected areas with neuralgia for several hours. Repeat twice a day.
The treatment regimen for a stiff trigeminal nerve:
- Warming up your feet before bed.
- Taking vitamin B tablets and a teaspoon of flower bee bread twice a day.
- Twice a day, smear the affected areas with the Vietnamese "Asterisk".
- Drink hot tea with soothing herbs at night (motherwort, lemon balm, chamomile).
- Sleep in a hat with rabbit fur.
When the pain affects the teeth and gums, chamomile infusion can be used. In a glass of boiling water, insist a teaspoon of chamomile for 10 minutes, then filter. It is necessary to take the tincture in your mouth and rinse until it cools. You can repeat the procedure several times a day.
What tinctures can treat the trigeminal nerve
- Hop cones. Pour raw materials with vodka (1: 4), leave for 14 days, shake daily. Drink 10 drops twice a day after meals. Must be diluted with water. To normalize sleep and calm the nervous system, you can stuff a pillow with hop cones.
- Garlic oil. This tool can be bought at a pharmacy. In order not to lose essential oils, you need to make an alcohol tincture: add a teaspoon of oil to a glass of vodka and wipe the whiskey with the resulting mixture twice a day. Continue the course of treatment until the seizures disappear.
- Althea root. To prepare the medicine, you need to add 4 teaspoons of raw materials to a glass of cooled boiled water. The agent is left for a day, in the evening gauze is moistened in it and applied to the affected areas. From above the gauze is covered with cellophane and a warm scarf. It is necessary to keep the compress for 1-2 hours, then wrap your face with a scarf for the night. Usually the pain stops after a week of treatment.
- Duckweed. This remedy is suitable for relieving swelling in trigeminal neuralgia. To prepare duckweed tincture, you need to have duckweed harvested in summer. Add a spoonful of raw materials to a glass of vodka, leave for a week in a dark place. The medium is filtered several times. Take 20 drops mixed with 50 ml of water three times a day until complete recovery.

It must be remembered that any folk remedies can only be additional measures treatment. Deny official medicine in favor of folk with trigeminal neuralgia is strongly not recommended. Since complications can be critical, a specialist should be consulted about each remedy used.
Prevention of facial neuralgia
There are no special precautions for trigeminal neuralgia because this condition rarely occurs due to external influences. But what actions can provoke an attack in patients who are guaranteed to have the disease is very clear. It is necessary to avoid aggressive impact on critical areas, sudden changes in temperature and wind.
The frequency of attacks of trigeminal neuralgia largely depends on the behavior of the patient himself. With an exacerbation of the condition, it is recommended to avoid hypothermia and drafts, increase stress resistance, balance the diet and strengthen the immune system in every possible way. It is very important to treat diseases of the oral and nasal cavity on time and to the end.
If there are attacks of severe pain in one half of the face, you should immediately contact a specialist and undergo an examination. Trigeminal neuralgia is handled by a neurologist. It is impossible to postpone treatment due to severe discomfort and the fact that the pathology can be a symptom of another disease.
Manifestation of trigeminal neuralgia
The sensations that the disease causes are quite painful. Eating, talking, and even the slightest breeze can cause pain. It is localized in the area of the eyes, nose, lips, teeth, gums, at certain points of the face (trigger zones, otherwise: exit points of the trigeminal nerve), and sometimes covers the entire surface of the skin of the face. The attack is intense, long. The disease lasts for years, and therefore many patients are covered by depression. Except pain autonomic symptoms occur: redness of the face, sweating, lacrimation, spasm of the facial muscles. Usually, all manifestations extend to one half of the face and patients try to cover it, not to chew on the affected side.
What is the trigeminal nerve?
The trigeminal nerve, as the name suggests, has three branches. All these branches are responsible for the sensitivity of the skin of the face and mouth: the first branch innervates the forehead, nose, and around the eyes; second: cheekbones, upper jaw, upper lip, third: lower lip, lower jaw. In addition to sensory fibers, the trigeminal nerve has so-called motor fibers that innervate the masticatory muscles. The branches of the nerve exit the skull through certain holes, by palpating which, the doctor can determine which of the branches is affected. These points are called trigger zones.
Causes of the disease
There are many causes for trigeminal neuralgia. Most of them are of a dental nature: poorly made prostheses, complex tooth extraction, osteomyelitis of the jaw bones, as well as inflammation of the sinuses, viral diseases(herpes, which often affects nervous system), multiple sclerosis, etc. But besides this, the cause may be in a neoplasm that compresses the branches of the nerve.
Treatment
They treat trigeminal neuralgia with medication, prescribing painkillers, anticonvulsants such as carbamazepine and finlepsin, antispasmodics, B vitamins, and antidepressants, because depressive states exacerbate and intensify the perception of pain.
In addition to drugs, not bad healing effect give physiotherapy: diadynamic currents, laser treatment, electrophoresis with hydrocortisone, ultrasound treatment.
As an extreme method, with inefficiency drug therapy surgical treatment is used, which is aimed at preventing the conduction of a nerve impulse. It is carried out by crossing or removing one of the branches of the trigeminal nerve. But the nerve tends to recover and the discomfort reappears.
Blockade
One of the effective drug treatments for neuralgia is blockade. It consists in the introduction of an anesthetic, which, as a rule, is a concentrated solution of novocaine (often with hydrocortisone) at the exit point of the trigeminal nerve branch. There are other anti-inflammatory drugs, such as diprospan blockade, but this blockade is more often used for joint pain. Only a doctor can evaluate and prescribe the best remedy to carry out the blockade.
To begin with, by probing the trigger points, they determine which of the branches of the nerve causes pain and then a solution is injected into this place: first intradermally, then into the subcutaneous fatty tissue to the bone. If the pain occurs due to the first branch, which innervates the skin of the forehead, nose and the area around the eyes, then the injection is made over the orbit. The second branch is "blocked" under the orbit, and the third at the corner mandible. Sometimes they make a blockade with an injection in the chin area, where one of the branches of the third branch, the mental nerve, comes out.
Intercostal neuralgia in children
Intercostal neuralgia is a neurological disease affecting peripheral nerves. AT childhood this pathology is rare.
Pain in the right side under the ribs

Doctor A. Deryushev
So, pain on the right, under the ribs. What could it be? What is causing this pain? Let's discuss in more detail. On the right, under the rib, the liver is located, which means that most of the problems in this area can be associated with this organ. Inflammation of the liver tissue is called hepatitis - they are different - acute and chronic, viral and toxic.
Colic in babies - causes and treatment

Colic is quite common in babies. You can talk a lot about this, but for each individual parent, this phenomenon is a disaster. No adult can be calm in this situation, but you need to adequately help your child.
Intercostal neuralgia: how to relieve pain

Very often, if there is pain in the chest, first of all they think about heart problems and turn to a cardiologist. However, it often turns out that the matter is not in the heart, but in the intercostal nerves, which for some reason are compressed and irritated either by a pathologically altered spine or by tense muscles.
Incomplete blockade of the left leg of the bundle of His
When we are overcome by a cold with endless sneezing and coughing, almost everyone knows what to do. Someone brews lime blossom according to a grandmother's recipe, and someone goes to the pharmacy for the usual paracetamol or the advertised new miracle drug. However, many ordinary people are completely lost when the heart is under the gun of the disease.
Right ventricular block

It often happens that the terms of cardiologists and incomprehensible entries in the ECG description frighten and confuse patients, which leads to the appearance of non-existent diagnoses in everyday life. Blockade of the right ventricle of the heart is the wrong name for a completely different concept. Therefore, it will not be superfluous to clarify and understand the “blockades” and “ventricles”.
Left ventricular block

The heart muscle has special properties compared to other organs. human body. One of these properties is the conductivity of impulses that occur in special structures of the heart tissue. Sometimes it happens that the impulse is not transmitted by the cells of the heart. Such conditions are called blockades.
Sources
- http://NewVrach.ru/blokada-trojnichnogo-nerva.html
- https://CreateSmile.ru/trojnichnyj-nerv/
- http://hirurgs.ru/content/blokada-troinichnogo-nerva
novocaine trigeminal nerve block used to relieve intense pain in neuritis or trigeminal neuralgia. First, pain points (Valle points) are set, with pressure on which an attack of pain most often begins. Depending on this, the injection site is chosen. A concentrated solution of novocaine (1-2%) or a mixture of it with hydrocortisone (25-30 mg per injection) is injected.
Blockade of the 1st branch of the trigeminal nerve. To determine the place of insertion of the needle II with the finger of the left hand, divide the upper edge of the orbit in half and, without removing the finger, put the II finger of the other hand inside it immediately above the eyebrow. Here you can feel the supraorbital opening, or supraorbital canal. Above it, 1-1.5 ml of a 2% solution of novocaine is injected intradermally with a thin needle and then, introducing an additional 2-3 ml, the subcutaneous tissue and tissues are infiltrated to the bone around this hole.
After contact with a bone, the needle can be immersed into the depth of the canal by no more than 5-6 mm. When blockade with hydrocortisone, it is also administered after preliminary intradermal anesthesia with a solution of novocaine.
Blockade of the II branch of the trigeminal nerve in the region of the infraorbital foramen. Determine the middle of the lower edge of the orbit. In this case, it is better to put the second finger of the brush on top so that the pulp of the nail phalanx rests on the edge of the orbit. Departing 1.5-2 cm down from this place, novocaine solution is injected intradermally and then the underlying tissues are infiltrated towards the infraorbital foramen and around it, up to the bone. Enter 3-4 ml of a 2% solution of novocaine. In this case, as in the blockade of the 1st branch, a thick and short needle is used. The most correct direction of the needle is slightly upward and outward, so that its pavilion almost comes close to the wing of the nose. Do not strongly press the needle on the bone and advance the needle after contact with it by more than 0.5 cm.
Summing up solution novocaine to the infraorbital nerve at the infraorbital foramen can also be performed according to the method of V.F. Voyno-Yasenetsky (1946).
Blockade of the III branch of the trigeminal nerve at the angle of the lower jaw. The patient lies on his back, with a roller under the shoulder blades. The head is thrown back and turned in the opposite direction. After intradermal anesthesia, a thin needle 5-10 cm long is inserted at the lower edge of the lower jaw, retreating from the angle of the jaw anteriorly by 2 cm. The needle should slide along the inner surface of the jaw parallel to its ascending branch. At a depth of 3-4 cm, the end of the needle approaches the area where the mandibular nerve enters the thickness of the jaw through the mandibular foramen. 5-6 ml of a 2% solution of novocaine is injected here.
mental nerve block produced on the lower jaw at the exit of this nerve through the mental foramen. In order to locate this foramen, it is useful to consider that the supraorbital, infraorbital, and mental foramen are in the same vertical line. It is not difficult to determine the mental foramen, given that it is located under the alveolar septum between the I and II premolars or under the alveolus of the II premolar, and it is located exactly in the middle of the distance between the alveolar edge and the lower edge of the jaw. The needle can be inserted both through the skin and through the mucous membrane of the vestibule of the mouth.
In addition to the introduction novocaine and hydrocortisone, with trigeminal neuralgia, perineural administration of vitamin B12 is used. A significant improvement in the condition of patients comes from supraorbital injections of this vitamin (in doses of 1000-5000 μg per injection) in the region of the I branch of the trigeminal nerve, regardless of which branch the pain attack begins from. Elongation of pain-free intervals is also achieved by general effects that complement the antalgic effect of the blockade, as mentioned above.
Some forms trigeminalgia etiologically closely related to diseases of the paranasal sinuses. Therefore, with neuralgia of the pterygopalatine node (Slader's neuralgia), lubrication of the posterior parts of the nasal cavity with a 2% solution of cocaine and instillation of a 3% solution of ephedrine into the nose (3 drops 3 times a day) are additionally prescribed.
Educational video on the anatomy of the trigeminal nerve and its branches
In case of problems with viewing, download the video from the pageA. Indications. Blockade of the facial nerve is indicated for spasms of the facial muscles, as well as for herpetic nerve damage. In addition, it is used in some ophthalmic operations (see Chapter 38).
B. Anatomy. The facial nerve leaves the cranial cavity through the stylomastoid foramen, in which it is blocked. The facial nerve provides taste sensitivity to the anterior two-thirds of the tongue, as well as the general sensitivity of the tympanic membrane, the outer ear canal, soft palate and part of the pharynx.
The point of insertion of the needle is immediately anterior to the mastoid process, below the external auditory meatus and at the level of the middle of the mandibular branch (see Chapter 38).
The nerve is located at a depth of 1-2 cm and is blocked by the introduction of 2-3 ml of local anesthetic into the region of the stylomastoid foramen.
G. Complications. If the needle is inserted too deep, there is a risk of blockage of the glossopharyngeal and vagus nerve. Careful aspiration testing is essential, as facial nerve located in close proximity to the carotid artery and internal jugular vein.
Glossopharyngeal nerve block
A. Indications. Blockade of the glossopharyngeal nerve is indicated for pain caused by the spread of a malignant tumor to the base of the tongue, epiglottis, palatine tonsils. In addition, the blockade makes it possible to differentiate neuralgia of the glossopharyngeal nerve from trigeminal neuralgia and neuralgia caused by damage to the knee node.
B. Anatomy. The glossopharyngeal nerve exits the cranial cavity through the jugular foramen medially to the styloid process and then passes in an anteromedial direction, innervating the posterior third of the tongue, muscles, and pharyngeal mucosa. The vagus nerve and accessory nerve also leave the cranial cavity through the jugular foramen, passing near the glossopharyngeal nerve; close to them carotid artery and the internal jugular vein.
B. The technique of performing the blockade. A 22 G, 5 cm long needle is used, which is inserted just behind the angle of the mandible (Fig. 18-5).
Rice. 18-5. Glossopharyngeal nerve block
The nerve is located at a depth of 3-4 cm, nerve stimulation allows you to more accurately orient the needle. Inject 2 ml of anesthetic solution. Alternative access is carried out from a point located in the middle between the mastoid process and the angle of the mandible, above the styloid process; the nerve is located immediately anterior to the styloid process.
G. Complications. Complications include dysphagia and vagus nerve block leading to ipsilateral vocal cord paralysis and tachycardia, respectively. Blockade of the accessory and hypoglossal nerves causes ipsilateral paralysis of the trapezius muscle and tongue, respectively. Performing an aspiration test prevents intravascular injection of anesthetic.
Occipital nerve block
A. Indications. An occipital nerve block is indicated for the diagnosis and treatment of occipital headache and occipital neuralgia.
Rice. 18-6. Occipital nerve block
B. Anatomy. The greater occipital nerve is formed by the posterior branches of the C 2 and C 3 cervical spinal nerves, while the lesser occipital nerve is formed from the anterior branches of these same nerves.
B. The technique of performing the blockade. The greater occipital nerve is blocked by injecting 5 ml of an anesthetic solution approximately 3 cm lateral to the occipital protuberance at the level of the superior nuchal line (Fig. 18-6). The nerve is located medial to the occipital artery, which can often be palpated. The small occipital nerve is blocked by the introduction of 2-3 ml of anesthetic even more lateral along the upper nuchal line.
G. Complications. There is a slight risk of intravascular injection.
- How to anesthetize the trigeminal nerve?
- Blockade of the first branch of the trigeminal nerve
- Retrobulbar blockade
- Blockade of the second branch of the trigeminal nerve
- Intraorbital blockade of the second branch of the trigeminal nerve according to Hartel
- Complications
- Blockade of the second branch of the trigeminal nerve according to Brown
- Peculiarities
- Intraorbital blockade of the second branch of the trigeminal nerve according to Hartel
- Blockade of the third branch of the trigeminal nerve
- Brown mandibular nerve block
- Technique
- Blockade of the mandibular nerve according to Hartel
- Peculiarities
- Brown mandibular nerve block
- Blockade of the first branch of the trigeminal nerve
The emergence and development of such an important method of anesthesia as blockade of the cranial nerves is based on the experiments of alcoholization of the trigeminal nerve and partly in the Gasser ganglion (this is the ganglion Gasseri), with neuralgia, produced by Schlosser, Ostwalt, Wright, Bodin, Keller and others. These experiments served as the basis for the blockade of the trigeminal nerve and for deep injections into separate branches of n. trigeminus at the base of the skull, up to and including the Gasser node. Braun, Peuckert, Offerhaus and Hartel developed the technique for this valuable method of anesthesia, but also worked on this issue elsewhere: Georg Hirschel simultaneously reported several successful trigeminal nerve blockades at the Heidelberg Surgical Clinic.
At the beginning of the 20th century, extensive experiments in this area were published, mainly by Hartel, and he is credited with the use of local anesthesia of the gasser node. Long ago local anesthesia, due to its extraordinary development, has become a special area requiring for correct execution sufficient experience, but now this experience is even more necessary, after the anesthesia of the trigeminal nerve and the Gasser ganglion has been separated to some extent into a special section of regional anesthesia. Without dexterity and experience in this area, reliable and safe anesthesia is impossible. This certainly requires a thorough knowledge of the course of the branches of the trigeminal nerve and their innervation of certain areas of the head. When learning to perform a blockade, it is hardly possible to do without a good model or skull, which sets the direction of the inserted needle and the depth to which it should penetrate.
How to anesthetize the trigeminal nerve?
Blockade of the first branch of the trigeminal nerve
The first branch of the trigeminal nerve - n. ophtalmicus is divided into three branches:
The blockade of these individual branches, according to the methods described by Brown and Peakert, consists in the injection of a local anesthetic, in particular novocaine, into the orbit, corresponding to the course of these nerves, outside the muscular cover of the eyeball - bulbus oculi.
Damage to the eyeball is easy to avoid if you follow the proposed rules. For this, straight long needles are used; the use of curved varieties, as recommended by some, is not necessary, and Brown warned against this as early as the beginning of the 20th century. Injection into individual nerve endings of the first branch of the trigeminal nerve is performed exactly in those places where, according to the anatomical structure of the bony cavity of the orbit, there are the best and most reliable ways for passing the needle. The point of the latter must penetrate into the orbit when guiding over the bone, and this is only possible where the bony wall of the orbit is flatter and not too concave. Such places are located on the lateral and on the upper part of the medial wall of the orbit; on its lower wall there is also a mostly flat bone surface, so that a blockade can also be carried out here. The photo below shows the inserted needles for medial and lateral orbital injections.
 Medial and lateral orbital injections
Medial and lateral orbital injections
Medial injection anesthetizes the branches of n. nasociliaris and nn. ethmoidales; lateral injection - n. frontalis and n. lacrymalis.
The injection points for these three orbital injections are shown in the photo below.
 Orbital injections
Orbital injections
Blockade of the first branch of the trigeminal nerve through lateral injection of the orbit
At the point "a", lying above the most lateral corner of the eye, a lateral injection is made, for anesthesia n. frontalis and n. lacrymalis.
According to Brown, a needle is injected at this point so that its tip, hitting the bone, does not leave the bone anymore, and then the needle is inserted to a depth of 4½-5 cm to the fissura orbitalis super. Here they run into the upper wall of the orbit, so that further advancement of the tip is impossible. Brown here injects 5 ml of a 1% solution of novocaine with adrenaline into the circumference of fissura orbitalis superior; Hartel advises to penetrate to a maximum depth of 3 cm and only then inject a local anesthetic.
With this lateral injection of the orbit, anesthesia of the skin occurs at the lateral angle of the eye, at the medial angle of the eye, on the upper eyelid, on the forehead and crown; in addition, there is anesthesia of the conjunctiva of the lateral and medial part of the upper eyelid and part of the conjunctiva of the lower eyelid.
Blockade of the first branch of the trigeminal nerve through the medial injection of the orbit
With a medial injection of the orbit, for anesthesia nn. ethmoidales the point of injection will be point "b". It lies, according to Brown, a finger above the inner corner of the eye (see photo above).
The needle is inserted here, under the control of palpation with the tip of the bone, to a depth of 4-5 cm in the horizontal direction. Brown injects here 5 ml of a 1% solution of novocaine with adrenaline, calculated on the medial and upper wall of the orbit.
According to Hartel for blockade n. ethmoidalis ant., which innervates the upper and anterior part of the nasal mucosa and the skin of the tip of the nose, the needle should be inserted about 2 cm deep. This depth is not enough to reach n. ethmoidalis post., which supplies the posterior cells of the ethmoid bone and the cavity of the sphenoid. Since with a deeper injection in the direction of the foramen ethmoidale post, they get too close to the optic nerve, Hartel suggests making a medial injection of the orbit, no deeper than 3 cm, counting on the diffusion of the solution to a greater depth.
After injection into the orbit, Brown's experience shows a rapidly passing protrusio bulbi with swelling of the upper eyelid. There are no complications. Since the injection of the orbit is carried out according to Brown along the bone wall outside the circulus tendineus and the muscle funnel of the bulbus oculi, the influence on n. opticus and on nn. ciliares was not observed. According to Kredel, in connection with the injection of the orbit, the appearance of amaurosis was noted, lasting about ten minutes. It could have been caused by adrenaline or by the local anesthetic itself. Voyno-Yasenetsky observed passing amaurosis, which occurred only a day after the operation and was caused by inflammatory edema of the orbit. This case must be considered as a consequence of local anesthesia for frontal sinus empyema.
Retrobulbar blockade
For anesthesia of the eyeball during enucleation or exenteration, it is necessary to produce a retrobulbar blockade of nn. ciliares and ggl. ciliare.
Lowenstein for this purpose injected a needle at the middle of the lateral edge of the orbit, to a depth of 4½ cm into the orbit, between the eyeball and the conjunctiva; here he turned the needle to the medial side, approached n. opticus and ganglion ciliare. He injected here 1 ml of a 1% solution of cocaine with adrenaline. Next, he injected ½ ml of the same solution around the eyeball.
Siegrist injected with curved needles retrobulbar tissue in a circle, from four conjunctival injection points.
Mende for retrobulbar blockade recommended inserting a needle behind the eyeball from two injection points, temporal and nasal, near the entry point of the optic nerve and nn. ciliares; he injected about 2 ml of a 1 or 2% solution of novocaine with adrenaline. In addition, 1 ml of the same solution was injected subconjunctivally near the site of attachment of the rectus muscle.
Seidel injected 1-2 ml of a 1% solution of novocaine with adrenaline subconjunctivally, around the eyeball. Then he injected from four points 1 ml of the solution retrobulbar through the conjunctiva and 1 ml of the same solution during the penetration of the needle into the retrobulbar tissue.
Blockade of the second branch of the trigeminal nerve
The second branch of the trigeminal nerve - n. maxillaris, as it passes through the foramen rotundum at the base of the skull, can be reached with an injection needle in various ways. This nerve trunk runs horizontally from the foramen rotundum into the pterygopalatine fossa, which it passes towards the canalis infraorbitalis. Having passed this channel, it appears as n. infraorbitalis from the opening of the same name.
One can now get into the second branch of the trigeminal nerve at the foramen rotundum or in the intraorbital route, or as tried before, by inserting the needle under the zygomatic arch and advancing it along the posterior surface of the maxilla into the fossa pterygopalatina.
The orbital pathway, according to Hartel, was first proposed by Payer, but implemented and methodically developed first. Hartel calls this path "axial puncture foramen rotundum".
If on the skull, on the lateral part of the lower edge of the orbit, the needle is passed straight inward, then they enter through the fissura inferior into the canalis infraorbitalis, between the sphenoid bone and the upper jaw; at the end of this channel lies the foramen rotundum. First, the needle encounters some obstruction at the planum pterygoideum of the sphenoid bone.
If we now lead the needle along this obstacle up and in the middle, then the foramen rotundum is reached.
The distance of the foramen rotundum from the lower edge of the orbit is approximately 4-5 cm.
Since the foramen rotundum is very narrow and completely filled with n. maxillaris, the needle is strongly opposed and the injection requires sufficient pressure. If you get into the nerve, then the patient feels pain diverging along the area of \u200b\u200binnervation of the second branch of the trigeminal nerve.
Intraorbital blockade of the second branch of the trigeminal nerve according to Hartel  Orbital blockade of the second branch of the trigeminal nerve in the foramen rotundum
Orbital blockade of the second branch of the trigeminal nerve in the foramen rotundum
According to Hartel, the technique of intraorbital blockade n. maxillaris in the foramen rotundum is as follows:
The needle is inserted at the lower edge of the orbit, in the middle between the sutura zygomaticomaxillaris and the outer lower edge of the orbit. With the index finger of the left hand, the eyeball is pushed upward and the needle is passed between the finger and the lower wall of the orbit sagittally and horizontally inward until, after passing through the fissura orbitalis inferior, it stumbles at a depth of 4-5 cm on the planum pterigoideum of the sphenoid bone. From this bone obstacle, a passage is palpated in depth upwards and inward until complaints of pain radiating to area n appear. maxillaris. Having hit the foramen rotundum with a needle, it is carried out into it for a few more millimeters and injected at a certain pressure with ½ ml of a 2% solution of novocaine with adrenaline. With a successful injection, anesthesia of the entire area innervated by the second branch of the trigeminal nerve occurs immediately.
The direction of the inserted needle is shown in the photo above with an arrow.
Complications
With the right technique, damage to both the eyeball and n can be avoided. opticus, but according to Hartel, hematomas are possible. The orbital path to the second branch of the trigeminal nerve is passable only in 90% of the skulls.
Blockade of the second branch of the trigeminal nerve according to Brown  Blockade of the second branch of the trigeminal nerve in the foramen rotundum with an injection under the zygomatic arch
Blockade of the second branch of the trigeminal nerve in the foramen rotundum with an injection under the zygomatic arch
Blockade n. maxillaris in the fossa pterygopalatina from an injection point under the zygomatic arch was first performed by Matas in 1900. Schlosser used this method to alcoholize the trigeminal nerve in neuralgia, and Braun used this technique for local anesthesia.
According to Hartel, only in 33% of cases it is possible to penetrate this way with the tip of the needle into the foramen rotundum, in most cases the action of the blockade is explained by the penetration of the local anesthetic to the nerve through diffusion in the loose fatty tissue of the fossa pterygopalatina.
According to Brown, the blockade technique n. maxillaris from the lower edge of the zygomatic arch is as follows:
The needle is inserted under the lower angle of the zygomatic bone and moves inward and upward. It slides along the tuber maxillare and if it is too curved, then the injection point should be chosen more posteriorly. Sometimes the needle clings to the large wing of the sphenoid bone; then you need to carefully change direction. At a depth of 5-6 cm, they fall into the fossa on the nerve.
Brown injected 5 ml of a 1% solution of novocaine with adrenaline into this place with a slight advance and pulling of the needle. While pulling, he injected another 5 ml of the same solution behind the upper jaw to cause contraction of the branches of art. maxillaris. If you hit n correctly. maxillaris, the patient again feels widespread pain in the face. If the advancement of the needle along the tuber maxillare is difficult, then under some circumstances it is necessary to make a new injection, more under the middle of the zygomatic bone and drive a double dose of a solution of novocaine with adrenaline, that is, 10 ml of a 1% solution, so that the anesthetic can reach the nerve by diffusion.
In the photo above, the needle was inserted into the foramen rotundum from under the zygomatic arch; the arrow shows the direction.
Peculiarities
Before injection, it is recommended, as with all blockades of the branches of the trigeminal nerve, to first orientate yourself along the skull and outline the direction of the needle. The latter is easy to fix during anesthesia of the 2nd branch of the trigeminal nerve, a line that seems to be drawn from the 1st or 2nd small molar of the lower jaw, obliquely through the skull to the middle of the cranial cover.
Guiding this guide line (see photo above) is often very helpful to anesthesiologists. The technique of this method of approach to the foramen rotundum is comparatively simple, reliable, and therefore recommended by many specialists.
Ostwalf maxillary nerve block
It should also be mentioned about the method of anesthesia n. maxillaris according to Ostwalf, who injects the needle from the side of the oral cavity behind the last molar and advances it forward along the planum infratemporale, entering the fossa pterygoidea.
Maxillary nerve block by Offerhaus
The next method of anesthesia of the maxillary nerve is according to Offerhaus. He measures the distance between the middles of both zygomatic arches with a compass and, subtracting from the measurement obtained the distance between the upper alveolar processes behind the molars, determines how far the foramen rotundum is from its point of injection. The latter is located either above or below the middle of the zygomatic bone.
Blockade of the third branch of the trigeminal nerve
The third branch of the trigeminal nerve, the region of sensitive innervation of which has already been discussed in one of the articles on our website, goes to the base of the skull through the foramen ovale.
Ostwalt mandibular nerve block
Ostwalt, to make alcoholization of the trigeminal nerve, introduced an angled needle with the mouth open behind the third upper molar through m. pterygoideus and reached the foramen ovale.
Blockade of the mandibular nerve according to Schltisser
Schltisser uses, also for the purpose of alcoholization of the third branch n. trigeminus, another way. He inserts the needle at the front edge m. masseter, pierces the cheek and reaches the oral cavity. Here he gropes for the needle with a finger inserted into the mouth, and pushes it further, to the greater wing of the sphenoid bone. The point should now be a few millimeters from the foramen ovale. This method is so bad that if the blockade is performed incorrectly, the mucous membrane of the mouth can be pierced.
Brown mandibular nerve block
Harris, Alexander, Offerhaus and Braun take the transverse path to reach the foramen ovale.
According to Brown, the injection point lies under the middle of the zygomatic bone. The needle is advanced obliquely into the skull. And here it is best to have a model of the skull near you, on which the oblique direction is fixed with another needle.
The needle sticks up to proc. pterygoideus; its tip is now approximately 1 cm from the foramen ovale. The depth of the inserted needle is noted, and the latter is then extended to subcutaneous tissue, turns a small angle back and is introduced again to the same depth. Then its point is at the foramen ovale.
At the same moment, the patient feels pain extending into the lower jaw. At this point, Brown injected 5 ml of a solution of novocaine with adrenaline. This technique, used by Brown, is very easy to perform and reliable, but as Hartel pointed out, variations in the base of the skull can sometimes create obstacles.
Blockade of the mandibular nerve according to Hartel  Blockade of the third pair of the trigeminal nerve at the foramen ovale (dashed arrow indicates the tilt of the needle required to approach the ganglion). Blockade of the gasser node (ganglion Gasseri).
Blockade of the third pair of the trigeminal nerve at the foramen ovale (dashed arrow indicates the tilt of the needle required to approach the ganglion). Blockade of the gasser node (ganglion Gasseri).
Very noteworthy is the method of reaching the foramen ovale from the front, developed by Hartel and recommended for the blockade of the gasser ganglion (ganglion Gasseri). This method, similar to the Schltisser technique, was successfully used by the author for quite a long time. It differs from the Schltisser technique in that it avoids needle piercing of the oral mucosa. The cannula is passed to the tuber maxillae under the zygomatic bone along the cheek, at the height of the upper molars, between the ascending branch of the lower jaw and the tuber maxillare to the planum infratemporale. Hartel used this path to pass through the foramen ovale to the Gasser node.
This Hartel method, the same for the blockade of the third branch of the trigeminal nerve and the Gasser node, is as follows:
On the cheek, at the height of the alveolar margin of the second upper molar, under the zygomatic arch, a wide nodule is superimposed, so that the injection point can be slightly changed if desired. Here a long thin needle, about 10 cm long, is injected into the skin. The index finger of the left hand is inserted into the oral cavity; right hand controls the needle. With further advancement of the latter, the point passes between the edge of the lower jaw and the tuber maxillare. Due to the fact that the needle with the help of a finger inserted into the mouth goes around m. buccinator, the oral mucosa remains intact. If now the needle enters the fossa infratemporalis, then m. pterygoideus externus and reaches planum infratemporale.
The depth reached should be 5-6 cm. This place is easy to mark.
Peculiarities
It is best to measure the length of the needle before injection and test the distance on the skull. Immediately, the direction of the axis of the needle is set simultaneously. Without knowing this direction, it is impossible to get into the foramen ovale with certainty.
Hartel made a small movable pointer on his needle, which was fixed at any distance. Such an addition no doubt alleviates the entire blockade of the third branch of the trigeminal nerve, but it is not necessary.
It is very important to note, in addition to the depth, the direction of the needle being inserted. According to Hartel, when viewed from the front, the axis continued in the imagination passes through the pupil of the eye, the side of the same name. When viewed from the side, the needle points to the tuberculum articulare of the zygomatic arch, that is, the axis extended in the imagination passes through this point.
Arteria maxillaris interna crosses in fossa infratemporalis. The danger of injuring her or the consequences of accidental damage is not very great. When using thin needles and with direct skillful injection, there are no complications with the artery. Hartel and Georg Hirshel never observed hematomas in their practice.
Before advancing the needle from the fossa infratemporalis into the foramen ovale, in order to navigate relative to the depth of penetration, Hartel set the pointer on his needle 1.5 cm from the level of the skin at the injection site.
Optionally block n. mandibularis of the trigeminal nerve at the foramen ovale, without penetrating the bony canal to the gasser node, it is not necessary to insert the needle as steeply as described above, and it must be injected under the zygomatic arch in a more horizontal direction to the protuberantia occipitalis.
In the photo above, the needle is inserted under the zygomatic arch in the foramen ovale. The axis marked with an arrow points to protuberantia occipitalis externa. This direction is easy to mark on the skull and remember. The external injection point on the cheek is approximately 2.5 cm outward from the corner of the mouth.
Georg Hirshel by this method always reached with success the third branch of the trigeminal nerve in the foramen ovale. When viewed from the front, the direction of the needle is the same as in the method given by Hartel, the tip of the needle, which is elongated in the imagination, points to the pupil of the same eye (photo below).
 The direction of the needle in the blockade of the trigeminal nerve (n. mandibularis) in the foramen ovale (when viewed from the front)
The direction of the needle in the blockade of the trigeminal nerve (n. mandibularis) in the foramen ovale (when viewed from the front)
With the method of inserting the needle through the foramen ovale to the ganglion Gasseri, as described above by Hartel, the direction of the imaginary axis when viewed from the side is different. The needle has a steeper stroke, as seen in the photo here, where it is drawn as an arrow through the foramen ovale. Above, the direction leads more towards the crown of the skull, while below it leads, lengthening towards the foramen mentale of the lower jaw. This change in direction depends on anatomical structure bony canal for the third branch of the trigeminal nerve, which opens in a steeper direction.
To anesthetize the third branch of the trigeminal nerve, 5 ml of a 1-2% anesthetic solution is sufficient. If the needle hits the nerve correctly, the patient indicates pain extending to the tongue and lower jaw.