Small increase in the R wave in the chest leads. Weak r-wave progression what it is The most disappointing diagnosis: heart attack
Reversal of negative T waves in patients with acute myocardial infarction as a manifestation of false-negative ECG dynamics.
Kechker's syndrome occurs on the 2-5th day of myocardial infarction; is not associated with retrombosis and the appearance (intensification) of clinical signs of left ventricular failure. In other words, it's not a relapse myocardial infarction. The duration of the Kechker syndrome, as a rule, does not exceed 3 days. Subsequently, the ECG picture returns to the original: the T wave becomes negative or isoelectric. The reasons for this ECG pattern are unknown. I am impressed by the point of view that it is a manifestation of epistenocarditis pericarditis; however, characteristic pericardial pain is not observed in this syndrome. The correct interpretation of the Koechker syndrome avoids unnecessary medical interventions such as thrombolysis or PCI. Prevalence: ~1 in 50 cases of myocardial infarction.
(synonym: memory phenomenon) - non-specific changes in the final part of the ventricular complex (mainly the T wave) in spontaneous contractions that appear with prolonged artificial (artificial) right ventricular stimulation.

Artificial stimulation of the ventricles is accompanied by a violation of the geometry of their contraction. With more or less prolonged stimulation (from 2-3 months), changes in the QRS complex in the form of negative T waves in many ECG leads may appear in spontaneous contractions. This dynamic mimics ischemic changes. On the other hand, in the presence of truly anginal pain, this phenomenon makes it almost impossible to diagnose small-focal myocardial infarction. A correct interpretation of the Chaterier phenomenon allows avoiding unnecessary hospitalizations and unjustified medical interventions.
It is important to understand that the Shaterier phenomenon can appear not only against the background of prolonged artificial stimulation of the heart - this is the main reason, but not the only one. With chronic bundle branch block, with frequent ventricular extrasystole, or with the WPW phenomenon, the end part of the ventricular complex in normal contractions can also change - negative or low-amplitude T waves are formed.
Thus, any long-term violation of the geometry of ventricular contraction due to abnormal conduction of the intraventricular impulse may be accompanied by the Chaterrier phenomenon.
It was noticed that on the ECG of healthy people, the amplitude of the T wave in V6 is always greater than the amplitude of the T wave in V1 by about 1.5-2 times. Moreover, the polarity of the T wave in V1 does not matter. Violation of this relationship, when the amplitudes of the T waves in V1 and V6 "align" or T in V1 exceeds T in V6 is a deviation from the norm. This syndrome is most often observed in hypertension (sometimes it is the earliest sign of LV myocardial hypertrophy) and in various clinical forms ischemic heart disease. Also he can be early sign digitalis intoxication.



The clinical significance of this syndrome: allows you to suspect "not the norm" and, if necessary, continue the diagnostic search "from simple to complex".
In most cases, the amplitude of the R wave in the "right" chest leads increases, and by lead V3 it reaches at least 3 mm. In situations where the amplitude of the R wave in V3 is less than 3 mm, it is legitimate to talk about the syndrome of insufficient growth of the R wave from V1 to V3. This syndrome can be divided into 2 categories:
1. There are no other abnormalities on the ECG.
Norm variant (more often with hypersthenic constitution),
sign of LV myocardial hypertrophy,
Erroneous location of the chest electrodes (V1-V3) on the intercostal space above.
2. There are other abnormalities on the ECG.
Typical for the following clinical situations:
- myocardial infarction in the "move" (in this case, there will be an ECG dynamics characteristic of a heart attack in leads V1 -V3),
Postinfarction cardiosclerosis,
Severe LV myocardial hypertrophy with other ECG criteria for hypertrophy,
Blockade of the LBB (complete or incomplete), blockade of the anterior branch of the LBB,
- S-type of right ventricular hypertrophy (rare).




Difficulty in interpreting R-wave undergrowth syndrome from V1 to V3 occurs, as a rule, if it is diagnosed as an independent, asymptomatic ECG pattern, and there are no other abnormalities on the ECG. With correctly applied chest electrodes and the absence of any cardiac history, its main cause is moderate LV myocardial hypertrophy.
As you know, premature contraction of the heart is called extrasystole. The extra excitation coupling interval is shorter ( short) interval between major contractions. This is followed by a compensatory pause ( long), which is accompanied by a lengthening of cardiac refractoriness and an increase in its dispersion (refractoriness dispersion). In this connection, immediately after the postextrasystolic sinus contraction, there is a possibility of another extrasystole ( short) is the "product" of the dispersion of refractoriness. The mechanism of "repeated" extrasystole: re-enrty or early post-depolarization. Examples:
short-long-short in a patient with functional brady-dependent extrasystole, which in this case does not have a special clinical significance:
short-long-short in a patient with severe sleep apnea syndrome, obesity and hypertension 3 tbsp. As you can see, after a compensatory pause, a paired polymorphic ventricular extrasystole appeared. In this patient, the short-long-short phenomenon can trigger polymorphic ventricular tachycardia and lead to sudden death:
short-long-short in a patient with long QT syndrome: initiation of torsade de pointes VT. Sometimes with this syndrome, the short-long-short phenomenon is a prerequisite for the initiation of ventricular tachyarrhythmia:
In patients with functional extrasystole, the short-long-short phenomenon has no clinical significance; it only "facilitates" the occurrence of bradydependent extrasystole. In patients with severe organic heart disease and channelopathies, this phenomenon can initiate the launch of life-threatening ventricular arrhythmias.
This term refers to the period in the cardiac cycle during which the conduction of a premature impulse becomes impossible (or delayed), although impulses with less prematurity are conducted. Differences in refractoriness at different levels of the conduction system of the heart provide the electrophysiological basis for this phenomenon.
On the first ECG, we see an early atrial extrasystole carried out to the ventricles without aberration. On the second ECG, the clutch interval of the atrial extrasystole is longer, however, the extrasystole is carried out to the ventricles with a delay (aberration).
Basically, the "gap" phenomenon is encountered by specialists performing EPS of the heart.
- short cycle aberration (3rd phase block), which occurs when the refractory period of the AV junction increases, due to a sudden lengthening of the interval between two previous contractions. The longer the interval between contractions, the higher the likelihood of aberrant conduction (or blocking) of the next supraventricular impulse.
A classic example of the Ashman phenomenon in atrial fibrillation:
Ashman's phenomenon that arose after a post-extrasystolic compensatory pause:
Blocking of atrial extrasystoles that arose after spontaneous lengthening of the interval between sinus contractions:
The clinical significance of the Ashman phenomenon: its correct interpretation avoids overdiagnosis of a) ventricular extrasystole and b) organic conduction disturbances in the AV junction.
Continuously recurrent course of paroxysmal atrial fibrillation, when after the end of one attack, after 1-2 sinus contractions, a new paroxysm starts.
characteristic of vagus-dependent atrial fibrillation. On the one hand, the phenomenon reflects the high ectopic activity of the muscular couplings of the pulmonary veins, on the other hand, the high profibrillatory readiness of the atrial myocardium.
In addition to retrograde excitation of the atria, there is a possibility of penetration of the ventricular impulse into the AV connection to a different depth with its discharge (prolongation of refractoriness, blockade). As a result, subsequent supraventricular impulses (usually 1 to 3) will be delayed (aberrated) or blocked.
Latent VA conduction due to PVC, leading to functional AV block 1st stage:
Latent VA conduction due to PVC, leading to functional AV block 2nd stage:
Latent VA conduction due to PVC, accompanied by a postposed (displaced) compensatory pause:

Clinical Significance covert VA conduction: the correct interpretation of this phenomenon makes it possible to distinguish between functional AV blockades and organic ones.
In most people, the AV node is homogeneous. In some, the AV node is electrophysiologically divided into a zone of fast and slow conduction (dissociated). If a person is subjectively healthy, this phenomenon has no clinical significance. However, in some patients, dissociation of the AV node is accompanied by the development of paroxysms of nodal reciprocal AV tachycardia. The trigger for tachycardia is the supraventricular extrasystole, which is carried out along the fast path, and only retrograde along the slow path - the re-entry loop closes. The phenomenon of dissociation of the AV node is reliably established by EPS of the heart. However, on a routine ECG, signs of a dissociative disease can sometimes be detected.
Consider the following clinical case. A 30-year-old female patient complains of unmotivated palpitations. Performed daily monitoring of the ECG.
Fragment of an ECG - a variant of the norm:
ECG fragment - AV blockade 1 tbsp. against the background of sinus tachycardia - absolutely not typical for the norm:
ECG fragment - AV blockade 2 tbsp., Type 1. Draws attention to the "fast" lengthening P-R interval followed by a ventricular wave:
A one-time increase in the P-R interval by more than 80 ms makes one think about the dissociation of the AV node into zones with different impulse conduction rates. This is what we see in this example. Subsequently, the patient underwent EPS of the heart: AV-nodal reciprocal tachycardia was verified. Ablation of the slow pathway of the AV node was performed with a good clinical effect.
Thus, signs of dissociation of the AV node on the surface ECG (alternation of normal and prolonged P-R intervals; one-time increase in the P-R interval in the Wenckebach period by more than 80 ms) in combination with an arrhythmic history make it possible to establish a diagnosis with a high probability even before cardiac EPS.
For all the seemingly improbability of this phenomenon, it is not so rare. The Kent's bundle serves not only as an additional pathway for conducting an impulse from the atria to the ventricles, but is also capable of possessing automatism (spontaneous diastolic depolarization). Extrasystole from the bundle of Kent can be suspected when the ECG signs of the WPW phenomenon are combined with late diastolic ectopia, simulating ventricular extrasystole. In this case, the dilated ventricular complex is a continuous delta wave.
Consider the following clinical example. A 42-year-old woman complained of attacks of unmotivated palpitations. Conducted two-day ECG monitoring. On the first day of the study, about 500 "widened" ventricular complexes were registered, appearing in late diastole and disappearing with an increase in heart rate. At first glance, a harmless functional ventricular extrasystole. However, late diastolic ventricular extrasystole, being calcium-dependent, mainly appears against the background of tachysystole or immediately after its completion. In this case, late ventricular complexes are recorded at a normal heart rate and with bradycardia, which is already strange in itself.
The situation cleared up completely on the second day of monitoring, when signs of intermittent ventricular pre-excitation manifested. It became clear that the late diastolic ventricular complexes are nothing more than extrasystoles from the Kent bundle.
The clinical significance of extrasystole from the Kent bundle: the correct interpretation of this phenomenon allows us to exclude the diagnosis of ventricular extrasystole and direct the diagnostic and treatment process in the right direction.
It is observed with supraventricular tachyarrhythmias, especially with atrial fibrillation. The essence of the phenomenon lies in the fact that supraventricular impulses, arriving frequently and irregularly in the AV junction, penetrate it to different depths; discharge it before reaching the ventricles. As a result, 1) the conduction of subsequent supraventricular impulses slows down, 2) the replacing ectopic impulse slows down (drops out).
On the surface ECG, the phenomenon of latent AV conduction can be spoken of on the basis of the following signs:
Alternation of short and long R-R intervals in atrial fibrillation:
No slip complexes at excessively long intervals R-R with atrial fibrillation:
Absence of escape complexes at the moment of a multi-second pause during the restoration of sinus rhythm:
When regular atrial flutter changes into irregular or atrial fibrillation:
Extrasystole from the distal parts of the AV junction (the trunk of the bundle of His) is a type of ventricular extrasystole and is called "stem". I designate this kind of extrasystole as an arrhythmic phenomenon, firstly, due to its relative rarity, secondly, due to external similarity with typical parietal ventricular extrasystole, and thirdly, due to its refractoriness to traditional antiarrhythmic drugs.
Clinical and electrocardiographic signs of stem extrasystole: 1) the QRS complex more often has a supraventricular appearance, or is slightly broadened due to sporadic aberration or due to the proximity to the proximal section of one of the legs of the bundle of His; 2) retrograde atrial activation is not typical; 3) the clutch interval is variable, since the stem localization of the extrasystolic focus suggests calcium-dependent depolarization - that is, abnormal automatism; 4) absolute refractoriness to class I and III antiarrhythmics.
Examples:
With stem extrasystole, a good clinical effect can only be obtained with long-term use of class II or IV antiarrhythmic drugs.
- conduction of the impulse instead of its expected blockade (aberration).
Example #1:
Probable mechanism: The atrial impulse caught the LBB into its supernormal phase.
Example #2:
Probable mechanism: the magnitude of the spontaneous diastolic potential in the His-Purkinje system is maximum immediately after the end of the repolarization of the "sinus" contractions (in our case, they are expanded due to the blockade of the LBB), so early atrial impulses have the greatest chance for "normal" conduction.
Example #3 (reverse Ashman phenomenon):

Probable mechanism: phenomenon of "gap" (failure) in conduction; shortening of refractoriness with a change in the length of the previous cycle.
Sudden sinus pauses on the ECG are not always easy to interpret unambiguously. Sometimes, for the correct interpretation of the phenomenon, in addition to a thorough analysis of the cardiogram itself, a comprehensive clinical and anamnestic assessment is necessary. Examples:
Pauses in sinus arrhythmia can be so pronounced that there is a misconception about the presence of SA-blockade. It must be remembered that sinus arrhythmia is asymptomatic; it is characteristic mainly for young and middle-aged people, including subjectively healthy people; appears (intensifies) with bradycardia (often at night); the pauses themselves are never too long, thereby provoking the appearance of slipping complexes; cardioneurotic symptoms are a frequent clinical satellite.
Sinoatrial blockade of the 2nd degree:

It is necessary to find out what type of blockade: 1st or 2nd. This is a fundamental question, since the forecast is different. SA-blockade 2 tbsp., Type 1 often occurs at rest (especially at night) in young healthy individuals; in classical cases, it is preceded clinically and electrocardiographically by Wenkibach's periodicals; as a rule, the pause does not exceed twice the R-R interval of the preceding contractions; the presence of slipping complexes is not typical; no syncopal history.

SA-blockade of the 2nd degree, type 2 appears suddenly without Wenkibach's periodicals; often there is a concomitant organic myocardial lesion, detected instrumentally; in aged persons, without obvious changes in the heart during ECHO, the main cause is cardiosclerosis; the pause may be longer than twice the R-R interval of the preceding contractions; slipping complexes often occur; a syncope history or equivalent is characteristic.


Blocked atrial extrasystole:
As a rule, it causes difficulties in diagnosis only if the number of blocked extrasystoles is small, and the number of ordinary (non-blocked) does not exceed the statistical norm - this dulls the doctor's vigilance. Elementary care in the analysis of the ECG will reliably verify the blocked atrial extrasystole. In my experience, a very early blocked ectopic P wave always deforms the T wave to some extent, making it possible to diagnose this phenomenon without EPS.
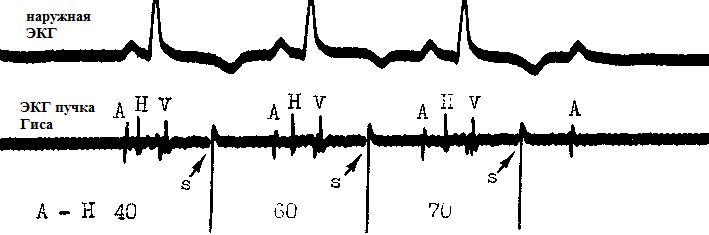
Mentioning the latent extrasystole in this section, I pay tribute to the extreme unusualness of this phenomenon. We are talking about stem extrasystole, which is blocked antero- and retrograde. Thus, it is not visible on the surface ECG. Its diagnosis is possible only with electrocardiography of the bundle of His. In the figure above, the stem extrasystole is provoked artificially: stimulus S. As you can see, the S stimuli do not propagate past the AV junction and therefore are not visible on the ECG. The third imposed stimulus causes transient AV blockade of the 2nd degree ("). On the external ECG, latent stem extrasystole can be suspected if there is a combination of conventional (wired) AV extrasystoles and sudden cardiac pauses of the AV blockade type 2 tbsp.
Aberration with increasing prematurity does not surprise anyone - since it is associated with a rapid increase in heart rate, when the refractoriness in the conducting system has not yet had time to shorten. Aberration looks much more unusual when the heart rate slows down, when it would seem that the refractory period is obviously over.

The basis for the long cycle aberration is the ability of the cells of the His-Purkinje system to spontaneous diastolic depolarization. Therefore, if there is a pause in the work of the heart, the membrane potential in some parts of the conduction system of the heart can reach the value of the resting potential ("critical hypopolarization"), which slows down or makes it impossible to conduct the next impulse. It should be understood that such a situation almost always reflects an organic pathology of the conduction system, when the cells of the AV junction are already initially in a state of hypopolarization (low value of the maximum diastolic potential). The phenomenon of brady-dependent blockade is not characteristic of a healthy heart and often precedes more severe conduction disturbances.
Literally means: the suppression of pacemakers by more frequent impulses. This phenomenon is based on the hyperpolarization of automatic cells due to the fact that they are activated more frequently than their own frequency of excitation. We can observe this physiological phenomenon on the ECG of any healthy person, when the sinus node subjugates all the downstream pacemakers. The higher the frequency of sinus rhythm, the less likely the occurrence of heterotopic impulses, including extrasystole. On the other hand, if the frequency of impulses of the ectopic focus exceeds the automatism of the sinus node, then the sinus node itself will undergo superfrequency suppression. The latter fact often attracts medical attention, since the pause after the restoration of sinus rhythm may be excessively long. For example:


When EFI through the phenomenon of "overdrive suppression" reveal dysfunction of the sinus node.
Early called ventricular extrasystole type R on T and atrial extrasystole type P on T.
With all the likelihood of the appearance of such extrasystoles in a healthy person (especially atrial ones), it must be remembered that the shorter the prematureness of extraexcitation, the less it is typical for normal myocardium. Therefore, when faced with early extrasystole for the first time, it is necessary to clinically and instrumentally assess the presence of myocardial refractoriness dispersion - that is, the likelihood of triggering tachyarrhythmia through extrasystole. Early atrial extrasystole, based on the muscular couplings of the mouths of the pulmonary veins, often begins to be detected in middle-aged people. Most often, it manifests by a reflex mechanism as part of an extracardiac disease due to wrong lifestyle. And if the cause of the arrhythmia is not eliminated, then sooner or later, early atrial extrasystole begins to trigger atrial fibrillation. The combination of early atrial premature beats, left atrial dilatation, and hypertension (or occult arterial hypertension) is the most reliable clinical predictor of future atrial tachyarrhythmias. In senile people, early atrial extrasystole is recorded in most cases.
A much greater responsibility falls on the shoulders of the doctor in the clinical analysis of early ventricular extrasystole - since life-threatening ventricular arrhythmias are almost always initiated by the phenomenon of R to T. In a healthy person, early ventricular extrasystole can be recorded only against the background of a frequent rhythm; with its contraction, it becomes mid-diastolic:
The isolated phenomenon of R on T in the background of normo- or bradycardia is always suspicious in relation to its special electrophysiological origin: early post-depolarization. As is known, there are no conditions for early post-depolarizations in a healthy myocardium (especially in the ventricular myocardium). Therefore, if the obvious causes of early ventricular extrasystole in the form of acute or chronic organic myocardial damage are rejected, it is necessary to exclude others - congenital ones. Let me remind you that with the so-called electrical heart disease, early ventricular extrasystole can be the only manifestation of latent pathology for a long time.
There is still no consensus on the origin of the U wave. The question of its clinical significance remains debatable. There are several theories of its origin:
1) The U wave is caused by late potentials that follow after their own action potentials.
2) The U wave is caused by potentials resulting from the stretching of the ventricular muscles during the period of rapid ventricular filling in the early phase of diastole.
3) The U wave is caused by potentials induced by delayed late repolarization during left ventricular wall stretch during diastole.
4) The U wave is due to repolarization of the papillary muscles or Purkinje fibers.
5) The U wave is caused by electrical oscillations caused by a mechanical wave of sufficient intensity at the mouths of the veins after passing through the normal arterial pulse along a closed "artery-vein" contour.
Thus, all theories are based on the existence of certain late oscillations, on a short time shifting the transmembrane potential of the myocardium at the time of early diastole towards hypopolarization. Theory number 2 is closer to me. A moderately hypopolarized myocardium has increased excitability - as you know, the U wave on the ECG chronologically coincides with the so-called supernormal phase of the cardiac cycle, in which, for example, extrasystole easily occurs.
Uncertain (and in my opinion insignificant) is the clinical significance of the U wave. Normally, the U wave is a small (about 1.5-2.5 mm on the ECG), positive, flat wave, following the T wave in 0.02-0.04 seconds. It is best visualized in leads V3, V4. Often, the U wave is not detected at all or “layers” on the T wave. And, for example, at a heart rate of more than 95-100 beats per minute, its detection is almost impossible due to superimposition on the atrial P wave. It is believed that normally it has the largest amplitude in healthy young adults. However, theoretically it can occur in any clinical situation, increasing in amplitude with tachysystole:

It is believed that the negative U wave is absolutely not characteristic of the norm. Negative U-oscillation is almost always associated with some kind of pathology. Another thing is that the diagnostic value of such a reversion can be completely different:
It is correct to speak about the replacing (“saving”) role of the ventricular rhythm only in those cases when it appears against the background of cardiac arrest in “paroxysmal” SA or AV blockades, or in passive AV dissociation. In other situations, we are dealing with an accelerated idioventricular rhythm (AVR), which appears as if unmotivated ("actively"). Its frequency does not exceed 110-120 per minute, otherwise ventricular tachycardia is diagnosed. There are several reasons for the emergence of the SIR:
Reperfusion syndrome in acute myocardial infarction,
Known organic heart disease with reduced systolic function of the left ventricle (as part of a potentially malignant Bigger ectopia),
digitalis intoxication,
Idiopathic cases in healthy individuals.
Most often, UIR appear in acute myocardial infarction at the time of complete or partial recanalization of the coronary artery. In such a situation, a large amount of calcium enters the stunned cardiomyocytes, which shifts the transmembrane potential to the threshold level (hypopolarization of the cell); as a result, cardiomyocytes acquire the property of automation. It is important to know that SIRs are not a reliable criterion for successful reperfusion: recanalization may be partial or intermittent. However, in combination with other clinical signs and the predictive value of UIR, as a marker of coronary blood flow recovery, is quite high. Cases of "reperfusion" ventricular fibrillation are very rare. Examples:
The reperfusion syndrome is faced mainly by doctors of the hospital stage working in cardioreanimation; polyclinic cardiologists or functional diagnostics physicians are more likely to deal with other causes of UIR.
Digitalis intoxication, as a cause of UIR, has become less and less common in recent years. It just needs to be remembered.
Of great clinical importance is the identification of UIR in patients with organic heart disease against the background of systolic dysfunction of the left ventricle. Any ventricular ectopia in such a situation should be treated as potentially malignant - it certainly increases the risk of sudden cardiac death through the initiation of ventricular fibrillation, especially if it occurs during the recovery period after exercise. Example:
Even 10-15 years ago, when registering UIR in people without organic heart disease, cardiologists issued a verdict of an "uncertain" clinical prognosis - such subjects were under medical patronage. However, long-term observations of them have shown that UIR does not increase the risk of sudden cardiac death and in such cases is a "cosmetic" arrhythmia. Often, UIR in healthy individuals is associated with other cardiac and non-cardiac anomalies: the WPW phenomenon, additional chords, early ventricular repolarization syndrome, manifestations connective tissue dysplasia syndrome. The clinical significance of UIR will be determined by the subjective tolerance of the arrhythmia and its effect on intracardiac hemodynamics (the likelihood of developing arrhythmogenic dilatation of the heart). Examples:

The physician should not be confused by such UIR parameters as frequency variability and polymorphism of ventricular complexes. The irregularity of the rhythm is determined by the internal automatism of the ectopic center or the blockade of the exit with Wenckebach's periodicals. The apparent polytopicity of ectopic complexes, in fact, is nothing more than aberrant conduction of excitation. According to the general opinion, the mechanism of UIR in healthy individuals is abnormal automatism.
In the differential diagnosis of accelerated ventricular rhythms, the Ashman phenomenon, the WPW phenomenon, and tachy- or brady-dependent bundle branch block should be excluded.
It is a variant of pacemaker hypersensing to the potentials of the skeletal muscles of the chest, shoulder girdle, abdominal muscles or diaphragm. As a result, the detecting electrode, perceiving extracardiac signals, gives a command to inhibit the next artificial impulse - a cardiac pause occurs, which can end in a faint for the patient. As a rule, myopotential inhibition is provoked by some actions, for example, active work with hands. This phenomenon is typical for pacemakers with a monopolar lead configuration; they have been implanted less and less in recent years. Examples:
Options for correcting myopotential inhibition: 1) decreasing the electrode sensitivity threshold, 2) reprogramming the system for a bipolar sensing version, 3) replacing the electrode with a new one, with a bipolar core.
As is known, the delta wave is a specific sign of ventricular preexcitation, due to the presence of an additional antegrade conduction pathway without the impulse delay characteristic of the AV node. The usual ECG picture in the form of a delta wave, expanding the QRS complex and shortening the P-Q interval due to preexcitation, is called the WPW phenomenon. However, sometimes there is a "temptation" to detect a delta wave where it actually does not exist, but there is a ventricular extrasystole, the beginning of which is very similar to preexcitation. This is the so-called pseudo-delta wave. A similar ventricular complex imitates a continuous delta wave (synonyms: continuous antidromic conduction, extrasystole from the bundle of Kent). Diagnostic difficulty occurs if a ventricular extrasystole with a pseudo-delta wave is registered on a standard ECG. When analyzing long-term ECG monitoring, everything falls into place: the WPW phenomenon with extrasystoles from the Kent bundle (solid delta wave) always will be combined with the presence of ventricular complexes with a true delta wave. On the contrary, when registering ventricular extrasystole with a pseudo-delta wave, the classic signs of the WPW phenomenon (including intermittent preexcitation) will not be detected. Examples:
According to the "width" of the pseudo-delta wave, one can judge the localization of the extrasystolic focus: endocardial or epicardial. The algorithm is as follows: 1) if the pseudo-delta wave is greater than 50 ms, then we can talk about the epicardial origin of PVC, 2) if the pseudo-delta wave is less than 50 ms, then pay attention to the shortest RS interval in the extrasystole on a 12-lead ECG : its duration less than 115 ms indicates endocardial localization of the focus, while with a duration of 115 ms or more, they proceed to the third step: the presence of a q-wave in lead aVL, 3) the presence of a q-wave in lead aVL indicates the epicardial origin of PVC, its absence - about endocardial. For example, in the ECG below, even according to the most rough calculations, the width of the pseudo-delta wave exceeds 50 ms:
The localization of the extrasystolic focus is of interest not only to invasive arrhythmologists: with frequent epicardial extrasystole, the risk of developing arrhythmogenic dilatation of the heart is much higher.
. With frequent heart rate myocardial energy resources are mobilized. If an episode of tachysystole lasts too long or the heart rate is extremely high, then intracellular metabolism is disturbed (cannot cope with the load) - transient myocardial dystrophy is formed. In such a case, after the end of tachycardia on the ECG, nonspecific changes in repolarization, called post-tachycardia syndrome, can be detected. Theoretically, after any tachycardia (sinus, supraventricular or ventricular) in recovery period manifestations of post-tachycardia syndrome may occur. In its classical form, it is a transient reversion of the T wave in the precordial leads. However practical experience shows that ECG changes following tachycardia may also affect the ST segment. Therefore, in clinical practice the following manifestations of post-tachycarditis syndrome occur:
Oblique-ascending depression of the S-T segment with upward bulge (like "systolic overload"),
- "slow" oblique-ascending depression of the S-T segment,
Negative T wave.
The duration of the post-tachycarditis syndrome is unpredictably variable: from several minutes to several days. With persistent sympathicotonia, manifestations of post-tachycardia syndrome can exist for months and years. A classic example is the juvenile type of ECG (negative T waves in leads V1-V3), characteristic of adolescents and young people with a labile psyche.
Let's briefly consider the options for post-tachycarditis syndrome.
Ascending S-T segment depression with upward bulge after tachycardia, as a rule, is formed in individuals with initial manifestations of left ventricular myocardial hypertrophy; in such patients, the standard resting ECG has completely normal parameters. The most pronounced depression is observed in leads V5, V6. Her appearance is familiar to everyone:

As a rule, within no more than an hour after an episode of tachycardia, the ECG returns to normal. If myocardial hypertrophy progresses, then the normalization of the ST segment is delayed for hours or even days, and subsequently the manifestations of systolic overload are "fixed" at rest.
"Slow" oblique-ascending depression of the S-T segment is rare. Most often, it appears after tachycardia against the background of functional myocardial disorders of the type of NCD.

Negative T wave is the most common variant of post-tachycardia syndrome. It is extremely non-specific. I will give three examples.
Negative T waves in the precordial leads in a 21-year-old boy (can be considered as a juvenile type of ECG) against the background of persistent sympathicotonia:

Negative T waves in the chest leads, formed after ventricular tachycardia:

Negative T waves in the chest leads, formed after supraventricular tachycardia:
Clinical Significance post-tachycardic syndrome is great! It is a common cause of unnecessary hospitalizations and medical examinations. Mimicking ischemic changes, especially in combination with cardial syndrome, posttachycarditis syndrome can "mimic" coronary pathology. Remember him! Good luck with your diagnosis!
Approximately 2/3 of people left leg bundle of His branches not into two branches, but into three: anterior, posterior and middle. Along the median branch, electrical excitation extends to the anterior part of the IVS and part of the anterior wall of the left ventricle.

Her isolated blockade is exclusively a rare event. However, if it happens, then part of the IVS and the anterior wall of the left ventricle are excited abnormally - from the side of the posterior and lateral walls of the left ventricle. As a result, in the horizontal plane, the total electrical vector will be directed forward, and in leads V1-V3, the formation of high R waves (qR, R or Rs complexes) is observed. This condition must be differentiated from:
WPW syndrome,
right ventricular hypertrophy,
Posterior-basal myocardial infarction,
Normal ECG of children of the first years of life, when, for natural reasons, the potentials of the right ventricle predominate.
Blockade of the median branch of the left branch of the bundle of His can occur both as part of a functional conduction disorder, and indirectly reflect, for example, an atherosclerotic lesion of the anterior descending artery, being a subclinical ECG marker of coronary artery disease.


The author of these lines is literally a couple of times in his professional activity met this violation of conduction. Let me give you one such observation. The following ECG pattern was verified in a patient against the background of severe retrosternal pain (Fig. A): oblique elevation of the ST segment in leads aVL, V2 and V3; anterior-upper semi-block and blockade of the median branch of the left leg of the bundle of His (high-amplitude R waves in leads V2, V3). Outside the attack, the ECG returned to normal (Fig. B).
On coronary angiography, a spasm of the anterior descending artery in the middle third was detected in the patient, which passed with intracoronary administration of nitrates; concentric coronary atherosclerosis was absent. Vasospastic angina was diagnosed. Thus, the blockade of the median branch appeared only at the time of an anginal attack, reflecting "deep" myocardial ischemia.
As is known, pacemaker syndrome may be provoked by a chronically existing disruption of the normal sequence of atrial and ventricular contractions, for example, due to ventriculoatrial conduction or inadequately long AV delay; or its manifestation is associated with hemodynamic non-equivalence of natural (own) heart contractions and imposed ones.
Pseudo-pacemaker syndrome is a hemodynamic disorder due to the presence of ventriculoatrial conduction or severe 1st degree AV block with clinical manifestations similar to the pacemaker syndrome, but in the absence of pacing. The development of this "pseudo-syndrome" is most often observed with a long-term AV blockade of the 1st stage, exceeding 350-400 ms, when electrocardiographically, the P wave begins to overlap the S-T interval of the previous ventricular complex; in this case, atrial systole occurs against the background of a closed mitral valve.
Let me give you a literary observation. The patient was admitted to the clinic with symptoms of CHF decompensation 4 years after the implantation of the pacemaker in the DDDR mode with a base stimulation frequency of 50 per minute. ECG revealed sinus rhythm with AV blockade 1 tbsp. duration about 600 ms:
The total percentage of atrial stimulation did not exceed 5%, ventricular - 7%. In dynamics, it was found that rare episodes of imposed rhythm or P-synchronous ventricular stimulation were interrupted by ventricular extrasystole, which was again followed by sinus rhythm with severe AV block of the 1st stage:
The operation algorithm of this pacemaker was such that after any ventricular contraction, an atrial refractory period of 450 ms was triggered, and the P wave appeared approximately 200 ms after the ventricular complex - that is, very early and therefore was not detected. This led to almost complete inhibition of ventricular pacing. In this case, it was necessary either to shorten the atrial refractory period, or to provoke the development of a complete AV block. This patient, in addition to the basic therapy for heart failure, was prescribed high doses of Verapamil, which, by blocking AV conduction, led to the fact that ventricular contractions became 100% imposed (P-synchronous stimulation). Medical AV blockade turned out to be a decisive factor - it made it possible to eliminate desynchronization in the contraction of the atria and ventricles, after which the phenomena of heart failure were stopped.
In this example, we see how a long-term pronounced AV blockade of 1 tbsp. may lead to the development of heart failure.
Sometimes with pseudo-pacemaker syndrome, you can observe the phenomenon of "jumping" P wave ( P-skipped) when, against the background of a pronounced slowdown in AV conduction, the P wave does not just “dissolve” in the QRS complex, but precedes it.
- change in the length of the RR interval under the influence of ventricular contraction in the absence of ventriculoatrial conduction. It is traditionally believed that this arrhythmia occurs when the number of sinus P waves exceeds the number of ventricular QRS complexes - that is, with AV blockade of the 2nd or 3rd degree. At the same time, the PP interval, which includes the QRS complex, becomes shorter than the PP interval free from ventricular contraction:

However, ventriculophase sinus arrhythmia can be observed with ventricular extrasystole, artificial ventricular stimulation. For example:
The most likely mechanism for this phenomenon is atrial stretch during ventricular systole, causing mechanical stimulation of the sinoauricular node.
In recent years, the clinical and electrocardiographic approach to the syndrome of early ventricular repolarization has undergone significant changes. According to the consensus opinion of experts, in the absence of clinical manifestations (paroxysms of polymorphic ventricular tachycardia or ventricular fibrillation), this syndrome is correctly called pattern of early ventricular repolarization, thus emphasizing its current goodness within the framework of a harmless ECG anomaly. Term syndrome RRG is recommended to use only in symptomatic patients suffering from syncope or suffering from sudden cardiac death through the mechanism of ventricular tachyarrhythmia. Given the exceptional rarity of this course of the GERD phenomenon (~ 1 per 10,000 people), the use of the term pattern should be considered not just a priority, but the only correct one.
Criteria for diagnosing the RGC pattern have become more stringent. It is erroneous to assume that the concave elevation of the S-T segment is one of the markers of GC.Subject to analysis only deformation of the descending part of the R wave: the presence of a notch (wave j) on it or its smoothness refers to the RRJ pattern. The distance from the isoline (the reference point is the position of the P-Q interval) to the top of the notch or the beginning of smoothness should be at least 1 mm in two or more consecutive standard ECG leads (excluding leads aVR, V1-V3); the width of the QRS complex should be less than 120 ms, and the calculation of the duration of the QRS is carried out only in leads where the RGC pattern is absent.


According to the criteria described above, only ECG #1 has a PGC pattern:
Unfortunately, there are still no reliable criteria for the potential malignancy of the RGC pattern and the possibility of its transition to the syndrome. However, in the presence of the following clinical signs, a subject with a pattern of PPJ should be under medical supervision:
Dynamic change in the elevation of the j point in the absence of a change in heart rate,
The presence of ventricular extrasystoles of the "R to T" type,
The presence of syncope, presumably different in clinical course from vasovagal (i.e. fainting like "suddenly I was on the floor"),
Unexplained death in a first-degree relative under 45 years of age with a documented pattern of GC
Presence of RRJ pattern in most leads (aVR, V1-V3 - not considered),
Transition of wave j into a horizontal or downward segment S-T.
To determine the nature of the S-T segment (ascending, horizontal or descending), the position of the Jt point and the point on the segment S-T, separated from it by 100 ms:
Detection of 2nd degree AV blockade type Mobits II is almost always an unfavorable prognostic sign, since its presence, firstly, reflects a conduction disorder distal to the AV node, and secondly, it often serves as a harbinger of the development of more severe dromotropic insufficiency, for example, complete AV blockade.
At the same time, in practical cardiology, there is a significant overdiagnosis of AV blockade of the 2nd stage. Mobitz II type. Consider situations that can mimic such a blockade - the so-called pseudo-Mobitz II (false AV block II degree type II):
Long AV nodal periodicals in AV block II degree type I;

Sudden transient increase in the tone of the vagus nerve;

Hidden ;

After ventricular extrasystole;

Syndrome W.P.W.;

Potential difference between adjacent areas of myocardial syncytium in the repolarization phase of the cardiac cycle. In a healthy myocardium, the dispersion of refractoriness is minimal, and its clinical significance tends to zero. Speaking about the presence of dispersion of myocardial refractoriness in a patient, we a priori imply a high risk of developing profibrillatory arrhythmia.
The development of a clinically significant dispersion of refractoriness is possible in 2 cases: 1) the presence of an organic heart disease with severe systolic dysfunction; 2) violations of ion transport (channelopathy, electrolyte imbalance). In both cases, the distribution of electrical excitation in all phases of the cardiac cycle will not be homogeneous, which means that at the time of repolarization (relative refractoriness), conditions arise for the emergence of a premature action potential - which is electrocardiographically equivalent to an extrasystolic contraction. The extrasystolic excitation front will be just as asynchronous, therefore, during repolarization, there is a high probability of the appearance of another extrasystole, etc., up to the decay of the next electrical wave into several waves and the development of fibrillatory activity in the atria or ventricles.
Example 1. In acute myocardial infarction, another PVC triggered polymorphic VT, which turned into VF:
Example 2. Patient with severe hypokalemia (1.7 mmol/l). "Giant" Q-T interval (~ 750 ms). Against this background, frequent polytopic ectopic contractions appear. High risk of developing ventricular fibrillation:

Refractoriness dispersion, although an electrophysiological concept, is more often used by clinicians in a descriptive sense as a marker of an increased risk of life-threatening ventricular tachyarrhythmias, verified on the basis of the presence of instrumental signs of left ventricular systolic dysfunction. With the exception of some disorders of ion transport, the dispersion of refractoriness does not have direct ECG manifestations.
Consultative and diagnostic center No. 6, Moscow
in the intensive care unit and intensive care observed a patient with chronic heart failure, atrial fibrillation and changes in the electrocardiogram, which could be caused by both postinfarction cardiosclerosis and improper placement of electrodes or dextrocardia.
Keywords: dextrocardia, ECG, heart failure, case report.
First identified dextrocardia and associated complexity of diagnostics at intensive care unit
A.V. Syrov
Moscow Internal Affairs Clinical Hospital
Consultative and Diagnostic Center №6, Moscow
The paper describes the case which took place at the emergency and intensive care unit. Patient with chronic heart failure, atrial fibrillation had specific changes of electrocardiogram, which might have been caused by post-infarction cardiosclerosis, incorrect application of electrodes or dextrocardia.
keywords: dextrocardia, ECG, heart failure, case report.
Patient M., 91 years old, was admitted to the intensive care unit with severe shortness of breath, dry cough. On admission, shortness of breath 28 respiratory movements in min. Moist rales in the lower parts of the lungs on both sides. Blood pressure 180/105 mm Hg. Art., heart rate 85-115 beats / min. Atrial fibrillation. She has a history of a permanent form of atrial fibrillation, long-term hypertension. An increase in dyspnea is noted throughout Last year. Within a month, there was a sharp increase in shortness of breath, the appearance of a dry cough.
Preliminary diagnosis: ischemic heart disease. Atrial fibrillation, permanent form. Hypertension 3 tbsp. Hypertonic heart. Acute decompensation of chronic heart failure.
The first electrocardiogram (ECG) revealed atrial fibrillation, Q waves in leads I, II, AVL, AVF, V2-V6 (Fig. 1).
With a previous myocardial infarction on the ECG, the most indicative change is the presence of pathological Q waves. The Q wave is considered pathological if its width is 0.04 s or more, and the depth is at least 25% of the amplitude of the R wave in the same lead. However, the absence of R waves in almost all leads is not typical for postinfarction changes, which are usually local.
If the ECG does not rule out postinfarction cardiosclerosis, then an echocardiographic study helps to assess the contractile function of the left ventricle. Violation of local contractility and a decrease in the ejection fraction of the left ventricle confirms the presence of postinfarction cardiosclerosis.
Incorrect placement of electrodes on the limbs is easy to determine by the aVR lead. The P and T waves in this lead should be negative, and the QRS complex is opposite to the QRS complex in lead II. In this case, the aVR lead fully complies with the above criteria and eliminates incorrect electrode placement.
With dextrocardia, the heart is located in the right half of the mediastinum, mirroring the normal location. The ECG shows a reverse configuration in both the limb and chest leads. When the chest leads are applied to the right of the sternum, in a mirror image of the usual location of the chest electrodes and the reverse location of the leads from the limbs, the ECG takes on its usual form.
When repeated taking an ECG The technique described above (the reverse arrangement of the electrodes, Fig. 2) showed the appearance of R waves in leads I, II, AVL, AVF, V5-V6, and an r wave in leads V2-V4. The second ECG shows atrial fibrillation and blockade of the anterior superior branching of the left branch of the His bundle and insufficient growth of R waves in the chest leads (the amplitude of the R waves in leads V1–V3 does not exceed 3 mm, the amplitude of the R wave in V3 is higher than the R wave in V2). The most common cause of insufficient growth of the R wave is left ventricular hypertrophy, however, it is not possible to completely exclude postinfarction cardiosclerosis by ECG.
Echocardiography revealed dextrocardia. Violations of local contractility of the myocardium was not detected. The left ventricle is hypertrophied (the thickness of the interventricular septum is 16 mm, the thickness of the posterior wall is 15 mm), systolic function is preserved (ejection fraction 55% according to Simpson), diastolic function is impaired. Atrial dilatation was detected.
Ultrasound examination also revealed dextroposition of the abdominal organs.
In this way, the initial ECG changes that occurred were due to dextrocardia. Insufficient growth of the R waves in the chest leads is not due to cicatricial changes, but to left ventricular hypertrophy. Increasing shortness of breath was due to chronic heart failure, which was confirmed by an increase in brain natriuretic peptide to 5 thousand ng/l. The cause of CHF was a violation of the diastolic function of the left ventricle (diastolic heart failure), arterial hypertension and atrial fibrillation.
The hospital was prescribed next treatment: ACE inhibitor(fosinopril 20 mg twice a day), beta-blocker (metoprolol succinate 50 mg once a day), diuretics (veroshpiron 50 mg once a day, furosemide 20 mg intravenously, then 20 mg orally once a day for a short period ), an anticoagulant (warfarin with a target INR of 2.0-3.0; the initial dose of the drug is 5 mg 1 time per day, the maintenance dose is 3.75 mg 1 time per day), a statin (atorvastatin 20 mg / day). The patient was discharged in a satisfactory condition. Shortness of breath during normal physical activity was not observed. Normosystole, heart rate 70–85 beats/min, blood pressure 120–135/70–65 mm Hg. Art.
Changes in the structure and metabolism of the myocardium, coronary arteries, and conduction system of the heart, which occur as the body ages, are inevitably reflected in the electrocardiogram. According to the literature and our observations, the features of the ECG of practically healthy elderly and senile people are:
- the correct sinus rhythm, the severity of respiratory arrhythmia decreases (the number of pacemaker cells that perform the function of automatism in the sinus node decreases - in patients older than 75 years, the sinoatrial node contains less than 10% of such cells; the sympathetic effect on the heart is weakened);
- sinus bradycardia. As a person ages, his heart rate decreases. The degree of increase in sinus rhythm during the transition of an elderly person from a horizontal to a vertical position, respiratory fluctuations in the rhythm, the response to the Valsalva maneuver and the chronotropic response to atropine also decrease. Asymptomatic sinus bradycardia in aging people is mostly a benign condition;
- deviation of the electrical axis of the heart (eos) to the left, despite the development of age-related emphysema, which indicates the predominant changes in the myocardium of the left ventricle. This is due to the development of left ventricular hypertrophy (LVH) with age, the development of sclerotic and dystrophic changes in the myocardium, as well as some rotation of the heart around the longitudinal axis;
- expansion, flattening and deformation of the P wave (conditions for the spread of excitation in the atria worsen);
- prolongation of the PQ interval up to 0.22 s (due to slowing of the atrioventricular conduction and the rate of propagation of excitation through the ventricular myocardium, which in turn is explained by degenerative changes in the cells of the conducting system);
- splitting, broadening up to 0.10 s and a decrease in the voltage of the QRS complex (the process of depolarization changes);
- a decrease in the amplitude of the T wave in all ECG leads, as a reflection of a decrease in the level of repolarization processes in the myocardium. However, in leads I, II, aVL, V 3-6 in physiologically aging people, it is always positive, and the ST segment is on the isoline;
- prolongation of the QT interval due to changes in the functional ability of the myocardium and a decrease in its contractility;
- from V 1 to V 3 leads, the amplitude of the r wave slightly increases, which makes it difficult to diagnose myocardial infarction of the interventricular septum in the elderly;
- horizontal dextrorotation is often noted (the S wave is recorded up to lead V 6) - as a result of emphysema, often observed at this age.
In older people, rhythm and conduction disturbances are often observed: extrasystole, atrial fibrillation, sick sinus syndrome, atrioventricular (AV) blockade and blockade of the bundle of His bundle (BPH).
Interpretation of the results of an ECG examination of persons of older age groups presents certain difficulties, requires an individual approach, taking into account the main diagnosis, concomitant diseases, their complications, taking medications, and should begin with familiarization with the patient's medical records.
One of the features of elderly and senile patients is polymorbidity, i.e. most of them have several diseases, each of which has its own specific manifestations, features of the course, complications, and a different prognosis. On average, 5-7 diseases, usually chronic, are detected in elderly patients over 60 years of age. The most common in different combinations and varying degrees of severity of clinical symptoms are: atherosclerotic lesions of the arteries of the heart and brain, arterial hypertension, chronic bronchitis, emphysema, chronic pyelonephritis, chronic gastritis, cholelithiasis, diabetes mellitus, arthrosis, osteochondrosis of the spine, obesity, oncological processes . All these diseases can cause certain changes in the electrocardiogram.
Thus, even in the absence of hypertension and coronary disease heart (CHD) diabetes there is a deviation of the electrical axis of the heart (eos) to the left and nonspecific disorders repolarization. At hypothyroidism sinus bradycardia, low-amplitude QRS complexes, smoothed or inverted T waves are detected, often prolongation of PQ and QT intervals, there may be a decrease in the ST segment. At hyperthyroidism on the ECG, mainly rhythm and conduction disturbances are noted: sinus tachycardia, atrial fibrillation, extrasystole, AV blockade, bundle branch blockade, the ST segment is shifted downward, flattening or inversion of the T wave is noted in a large number of leads, the QT interval is lengthened . Anemia accompanied by sinus tachycardia and changes in the final part of the ventricular complex (smoothness of the T wave and / or depression of the ST segment). Obesity often leads to a deviation of the EOS to the left, a decrease in voltage and a widening of the QRS complex, a decrease in the amplitude of the T wave, a tendency to sinus tachycardia is characteristic, left ventricular hypertrophy is possible, various disorders of atrioventricular and intraventricular conduction may occur . Cerebral vascular diseases accompanied by disturbances in the rhythm and process of repolarization with characteristic wide negative T waves. At hiatal hernia negative T waves may be recorded on the ECG, which sometimes requires differential diagnosis with myocardial infarction.
It should be borne in mind that under conditions of polymorbidity, a complex interweaving occurs various forms heart damage, which in turn makes it difficult to interpret the ECG data of patients of older age groups.
The main forms of heart damage and comorbidities in elderly and senile patients include: a combination of hypertension with chronic coronary heart disease (sometimes also with diabetes mellitus), chronic cor pulmonale with coronary artery disease, combined hypertrophy of both ventricles, dilatation of both atria, simultaneous or sequential the development of several foci of necrosis of different depths distant from each other, the layering of a fresh infarction on previous cicatricial changes of the same or contralateral localization, the development of intraventricular conduction disturbances against the background of previous hypertrophy of the left or right ventricle, often combined with various arrhythmias.
The interaction of several processes can be accompanied by:
- complete leveling of the signs characteristic of each of them, and then the ECG turns out to be normal, or changed due to purely non-specific shifts in the repolarization phase;
- a manifestation of only one full-fledged syndrome, characteristic of one of several processes, with total absence pathological signs characteristic of other processes;
- the appearance of individual components from possible syndromes;
— development different types blockade of the legs of the bundle of His, as an independent form of damage for ECG diagnostics, preventing the detection of key signs of the main processes.
So, for example, ECG changes observed in cor pulmonale (eos deviation to the right, hypertrophy of the right parts of the heart) in older patients, in contrast to young patients, are very rare. This is due to the simultaneous presence of left ventricular hypertrophy (LVH) due to age-related changes myocardium, developing atherosclerosis. ECG diagnosis of LVH is difficult due to a decrease in the amplitude of the teeth of the ventricular complex of an age-related and pathological nature and the presence of intraventricular conduction disturbances. So, with the attachment of the blockade of the anterior branch of the left RPG, ECG signs of left ventricular hypertrophy may disappear, with complete blockade of the left RPG, the diagnosis of left ventricular hypertrophy becomes almost impossible.
Under conditions of a decrease in the voltage of the ventricular complex teeth in elderly and senile patients, the characteristic defiguration of the ST segment and the T wave, the ratio of R waves in the left chest leads often becomes the only ECG sign of LVH. In patients with coronary artery disease, blockade of the left NPG often occurs, making it difficult to diagnose myocardial infarction.
The course of diseases in old age is usually dim, latent, often atypical, the disease is clinically manifested by small shifts in functions. Therefore, dynamic monitoring of patients is very important. Both in the general clinical examination and in the ECG examination, importance is attached to "small" symptoms, especially those found in dynamics, sometimes atypical in the light of the generally accepted assessment of changes. So, for example, previously formed negative T waves with fresh violations of the coronary circulation often give false positive dynamics, transforming into smoothed or positive T waves. Therefore, the dynamics of the indicators themselves - positive or negative, from the point of view of its formal assessment should be taken into account when deciding on the state of health old man. In this regard, it is necessary to familiarize the doctor with the patient's medical records in detail in order to compare this ECG with the ECG taken earlier and with clinical data. The patients themselves should be focused on maintaining the results of the ECG examination.
In the elderly, ECG changes in the same disease may be different, and at the same time, in different diseases, the same type of deviation may be recorded. So, in case of hypertension, a normal electrocardiogram, ECG signs of LV hypertrophy, blockade of the left NPG can be recorded. But, first of all, it concerns changes in the final part of the ventricular complex. So, the causes of changes in the ST segment and the T wave can be coronary artery disease, left ventricular hypertrophy, electrolyte disturbances, medication, cerebrovascular disorders, infectious processes, anemia, and others. At the same time, in 30-50% of patients with known coronary artery disease, the electrocardiogram may remain completely normal (including during an angina attack). Therefore, ECG changes must be compared with the clinic.
It must be remembered that the development of a particular syndrome at a later age often has a multifactorial origin and one symptom can be caused by several causes at the same time. So, a negative T wave in a patient with coronary artery disease, arterial hypertension, diabetes mellitus, obesity, hernia of the diaphragmatic opening of the diaphragm can be due to all causes at the same time, as well as medication. Given the above, in the absence of the possibility of clinical verification of changes in the final part of the ventricular complex, it is necessary to use the term "disturbance of the repolarization processes", especially since the doctors of functional diagnostics put the electrophysiological approach into the term "ischemia" and "damage", while practical doctors almost always invest in this term clinical content, which can cause a diagnostic error and iatrogenic. Such an approach to the conclusion on the electrocardiogram in the elderly is all the more justified because often in older patients the leading clinical manifestation of the disease is a symptom of damage to other systems involved in the pathological process, and the most common “mask” in diseases of other systems is the “cardiac mask”.
One of the urgent problems of modern cardiology in geriatrics is arrhythmias and heart block, since there are also some features of their clinical manifestations, diagnosis (including history taking, physical examination and various instrumental methods) and clinical and prognostic interpretation.
Many older people take medications, often at the same time several items (from 3-4 to 10 or more) and for a long time. Many medications affect the cardiovascular system, cause changes in the electrocardiogram. In older people, "drug-induced arrhythmia" is quite common. In them, more often than in young people, an arrhythmogenic effect of therapeutic doses of a number of medicines(cardiac glycosides, sympathomimetics, methylxanthines, peripheral vasodilators, diuretics, psychotropic drugs, glucocorticoids, etc.), antiarrhythmic drugs in much lower doses can cause various rhythm and conduction disturbances. Many pharmacological agents cause changes in the electrocardiogram.
For example, a nicotinic acid can cause tachycardia, arrhythmias (up to atrial fibrillation), tricyclic antidepressants - sinus tachycardia, expansion of the QRS complex, lengthening of the intervals of QRS, QT, blockade of the legs of the His bundle, arrhythmias (extrasystole, atrial fibrillation, supraventricular and ventricular tachycardia), phenothiazines - sinus tachycardia, prolongation of PQ and QT intervals, changes in the T wave, arrhythmias (up to ventricular tachycardia and ventricular fibrillation). Barbiturates they inhibit the automatism of the sinus node with the development of replacing ectopic rhythms, slow down AV conduction up to the development of complete AV blockade, reduce the ST segment, flatten the T waves, lengthen the QT interval. Approximately 40% of older people take tranquilizers and antidepressants. At a therapeutic dose cardiac glycosides cause prolongation of the PQ interval, shortening of the QT interval, ST segment depression, T wave change. When taking cardiac glycosides, almost all known arrhythmias can occur, including several various arrhythmias in the same patient. Diuretics, removing potassium, alter repolarization, can lead to ventricular arrhythmias. Isadrin, salbutamol, asthmapent can cause tachycardia, activate ectopic foci, are dangerous in terms of the development of ventricular fibrillation. Eufillin can cause tachycardia, extrasystole and other arrhythmias (up to fatal arrhythmias).
An increase in the duration of the QT interval is a factor contributing to the appearance of ventricular tachycardia of the "pirouette" type, which can transform into ventricular fibrillation. Long QT syndrome occurs much more frequently in the elderly than in young adults. This is due to more pronounced changes in the myocardium due to aging and the presence of coronary artery disease.
The effect of drugs on ECG elements
ECG changes | Medicines |
Increase heart rate Slow down heart rate Lengthen the PQ interval Widen the QRS Prolong the QT interval | Sympathomimetics (ephedrine, isadrine, alupent, berotek); Antispasmodics (theophylline, eufillin); Glucocorticoids, thyroidin; Diuretics (hypothiazid, furosemide); Antihypertensive drugs (hydralazine, captopril); Tricyclic antidepressants and some tranquilizers; Atropine, belloid, bellataminal; Others (caffeine, nicotinic acid, eleutherococcus, pantocrine) Antiarrhythmic drugs (beta-blockers, ethmozine, amiodarone, verapamil, diltiazem); cardiac glycosides; Antihypertensive drugs (reserpine, clonidine, methyldopa, prazosin); Others (dipyridamole, pilocarpine, opiates) Antiarrhythmic drugs (quinidine, novocainamide, disopyramide, lidocaine, aymalin, propafenone, etmosin, etatsizin, beta-blockers, amiodarone, sotalol, verapamil, diltiazem); cardiac glycosides; Antihypertensive drugs (reserpine, clonidine); tricyclic antidepressants; Others (adenosine, theophylline) Antiarrhythmic drugs (quinidine, novocainamide, disopyramide, aymalin, propafenone, ethmozine, ethacizine, amiodarone); Tricyclic antidepressants, phenothiazines Tricyclic antidepressants, phenothiazines; Antibiotics and sulfonamides (erythromycin, clarithromycin, azithromycin, spiramycin, bactrim, sulfamethoxazole), antifungal drugs(ketoconazole, fluconazole, itraconazole); Cardiovascular drugs (adrenaline, ephedrine, cavinton); Antihistamines (astemizole, terfenadine); Diuretics (except potassium-sparing); Others (adenosine, papaverine, probucol, droperidol, haloperidol, cocaine). |
Acquired long QT syndrome can be caused by various reasons:
- severe electrolyte disturbances: hypokalemia, hypomagnesemia, hypocalcemia (including those caused by diuretics);
- iatrogenic and chemical toxic effects: medicines, poisoning with organophosphorus compounds, mercury, lithium preparations;
- heart disease: myocardial ischemia, myocardial infarction, rheumatism, myocarditis, cardiomyopathy, mitral valve prolapse, severe bradycardia, 3rd degree AV blockade;
- pathologies of the central nervous system: subarachnoid hemorrhages, trauma, thrombosis, embolism, infection, brain tumors, conditions after resuscitation;
- other causes: hypothyroidism, chronic alcoholism, lung carcinoma, Kohn's syndrome, pheochromocytoma, hypothermia, vagotomy, starvation or protein-restricted diet.
The cause of acquired long QT syndrome in most cases is the use of antiarrhythmic drugs. Approximately 90% of cases of ventricular tachycardia of the "pirouette" type are associated with taking quinidine, novocainamide or disopyramide. Risk factors contributing to the occurrence of pirouette-type tachycardia while taking antiarrhythmic drugs are hypokalemia, hypomagnesemia, bradycardia, and the presence of myocardial pathology. For ventricular tachycardia of the "pirouette" type, the so-called pause-dependence is characteristic - an attack of ventricular PT begins after the previous pause. In the interictal period, long QT syndrome may present with bradycardia, QT prolongation, prominent U-waves, episodes of T-wave reshaping, insufficient shortening, or even prolongation of the QT interval during rhythm acceleration.
Prolongation of more than 25% of the initial level or the absolute duration of the QT interval of more than 500 ms due to medication requires the mandatory discontinuation of all drugs that can prolong the QT interval, correction of blood serum electrolytes. It is practically important to diagnose prolongation of the QT interval in spontaneous angina pectoris, myocardial infarction, arrhythmias, electrolyte disturbances, in the treatment of drugs capable of prolonging the QT interval.
Shortening of the QT interval is observed with hyperkalemia, hypercalcemia, treatment with digitalis preparations.
Chronic ischemic heart disease
In the diagnosis of coronary heart disease (CHD), a correctly collected anamnesis is of great importance. However, not only with an unclear clinical picture, especially with an atypical course of angina pectoris, but also with a certain, judging by the anamnesis, diagnosis, it is always necessary full examination sick. Currently, functional research methods are widely used to assess coronary circulation: ECG registration at rest, various stress tests, pharmacological tests, Holter ECG monitoring, echocardiography (including stress echocardiography), atrial pacing (including transesophageal), radioisotope methods, coronary angiography, etc. It should be noted that in elderly and senile patients, it is almost impossible to carry out many diagnostic methods and it is often sufficient to use an ECG taken at rest, 24-hour Holter monitoring and echocardiography. The methods are quite informative, not burdensome for the patient, have no contraindications, and are available for practical healthcare.
Resting ECG often uninformative - even in patients with angina III-IV FC ECG may be normal. However, the ECG may show signs of coronary artery disease, such as a past myocardial infarction (MI) or the pathological nature of myocardial repolarization. Interpretation of changes in the terminal part of the ventricular ECG complex in elderly people is especially difficult due to a combination of age-related and pathological changes. Resting ECG may also reveal cardiac hypertrophy, bundle branch block (BBB), rhythm and conduction disturbances. Such information may be useful in determining the mechanisms responsible for the occurrence of pain in chest, or when identifying subgroups of patients with an increased risk of myocardial infarction or death.
ECG picture at the height of an anginal attack depends on the localization of the ischemic zone, the prevalence and duration of the process. There may be the following changes:
- depression of the ST segment more than 1 mm in two or more leads;
- displacement of the ST segment upward from the isolium of at least 1 mm;
- symmetrical inversion of T waves with a depth of more than 1 mm;
- flattening of the T waves;
- “pseudonormalization” of T waves;
- occasionally - an increase in T waves;
- transient blockade of the legs of the bundle of His, AV blockade, arrhythmias.
The ECG changes only at the height of an anginal attack, normalizing after it rather quickly, more often within 20 minutes, but not later than 1-2 hours. However, there is no clear parallelism between the displacement of the ST segment and pain attacks: at the height of an anginal attack, there is not always a displacement of the ST segment, and against the background of ischemic displacement of the ST segment, pain does not always occur. Thus, the absence of ECG changes during an angina attack does not exclude the diagnosis of coronary heart disease.
In elderly and senile patients, it is extremely careful to interpret ECG changes during an angina attack in order not to miss myocardial infarction. The assignment of ST segment depression due to an angina attack is justified only after a second ECG recording, when the attack was stopped, and the electrocardiogram returned to normal completely or became the original one.
Even more cautious should be treated in the elderly to the rise of the ST segment on the ECG and the diagnosis of "spontaneous angina". Prinzmetal's angina in older age groups is very rare, as the coronary arteries become rigid and spasm cannot occur in them. During an attack of Prinzmetal's angina pectoris, so-called "transient" Q waves may appear (due to a short-term cessation of electrophysiological processes in the ischemic myocardium). Spontaneous angina differs from myocardial infarction by rapid normalization of the ECG (within 20-30 minutes). Re-registration of the ECG after the end of an anginal attack is required.
In the diagnosis of angina pectoris, the results of stress tests are more informative, but they are often impossible in elderly patients due to concomitant diseases of the musculoskeletal system, limb vessels, neurological disorders, respiratory failure, ECG changes (rhythm and conduction disturbances). The informativeness of the test in elderly patients is reduced due to a more pronounced hypertensive response to physical activity, frequent appearances extrasystoles and other rhythm disturbances, muscle fatigue, which does not allow reaching threshold loads.
The value of the Holter ECG monitoring method lies in the ability to detect transient myocardial ischemia in everyday life. The method is especially useful for detecting episodes of vasospastic ischemia, asymptomatic myocardial ischemia and episodes of rhythm disturbance, which is especially important for the elderly and senile.
The role of echocardiography is great, in which calcification is detected coronary arteries, transient zones of myocardial hypokinesia, decreased ejection fraction .
Myocardial infarction (MI)
Elderly people are most difficult ECG diagnosis of MI (both acute and cicatricial stages). Percent diagnostic errors with MI in the elderly is from 28 to 42%. This is due to the following factors complicating diagnosis: frequent atypism of the clinic, recurrence of MI (45%), a high level of untimely treatment of patients for medical care (up to 40%), a high percentage of MI without a Q wave (up to 77%), a number of features ECG diagnostics MI in the elderly and senile.
The clinical and electrocardiographic picture of MI in elderly and senile patients has a number of features:
- MI in the elderly rarely begins with a typical anginal picture. In patients older than 60 years, arrhythmic, asthmatic, gastralgic, cerebral, peripheral, asymptomatic forms of myocardial infarction are more common. The painless form of MI in the elderly often occurs with diabetes mellitus, it can be manifested by "unmotivated" weakness, headache, dizziness, slight shortness of breath, nausea, and decompensation of diabetes. Asymptomatic forms of MI are more often detected by chance during preventive examinations (“ECG-finding”).
Arrhythmic variant of MI . The leading symptoms are symptoms of rhythm or conduction disturbances (more often paroxysmal tachycardias, less often - atrial fibrillation, AV blockade, blockade of the legs of the bundle of His), pain is mild. ECG signs of MI are masked by arrhythmia.
Asthmatic variant of MI manifested by shortness of breath and a clinic of cardiac asthma. The asthmatic variant of the onset of MI usually occurs with extensive MI, often repeated (especially if repeated MI develops soon after the previous one), in patients with heart failure, arterial hypertension.
gastralgic variant observed in hypertensive patients with severe atherosclerosis, with repeated MI, as well as in patients who have a combination of angina pectoris with peptic ulcer or cholecystitis, often occurs with lower localization of necrosis. The pain is localized in the epigastric region, accompanied by nausea, vomiting, bloating, muscle tension abdominal wall. In some diseases (acute pancreatitis, acute cholecystitis, appendicitis, perforated stomach ulcer or 12 p.c.), heart attack-like changes appear on the ECG. It can be extremely difficult to diagnose situations when MI is combined with any of the above diseases of the abdominal organs.
cerebral form. Her clinic is dominated brain symptoms- headache, dizziness, motor and sensory disorders, confusion, anginal syndrome, as a rule, is not expressed. In this case, the diagnosis of "impaired cerebral circulation" is very often made. In patients with a primary violation of cerebral circulation on the ECG, heart attack-like changes are often recorded. It is not always easy to determine which link is broken primarily and which is secondary. In addition, heart attack and stroke in the elderly are not alternative diagnoses, they are often combined. In individuals with severe atherosclerosis of the cerebral artery, thrombosis (or spasm) of the cerebral artery may occur simultaneously with MI. Patients with BMNC may experience subendocardial hemorrhage and myocardial infarction. MI develops in more than 20% of patients with acute stroke. MI is the most common cause of death from weeks 1 to 4 of a stroke.
- characteristic of MI in the elderly is a delay in the development of ECG changes in relation to clinical symptoms - signs of MI on the ECG may appear within a week after the development of a heart attack. More often normal ECG at the beginning of MI, it appears with damage to the lateral and posterior walls of the left ventricle.
- a feature of MI in the elderly is a high percentage of MI without a Q wave and a frequent lack of staging (ST segment elevation, formation of a Q wave and a negative T wave) and slow ECG dynamics. Difficulties arise in the diagnosis of small-focal MI, since often there is no displacement of the ST segment and the changes mainly concern the T wave.
- in patients old age more often there are lesions of the subendocardial, basal, lower parts of the left ventricle, the ECG diagnosis of which is difficult.
- the course of MI in elderly patients is often protracted - there is a slow dynamics of clinical symptoms, laboratory parameters, ECG data. The protracted course of myocardial infarction is often combined with a recurrent course. This requires constant dynamic ECG monitoring of patients.
- myocardial infarction in elderly patients is often accompanied by angina attacks, which is associated with the presence of chronic coronary insufficiency. Postinfarction angina may occur immediately after the cessation of acute anginal pain. Therefore, differential diagnosis is often required between angina attacks and recurrent MI, i.e. Elderly patients need to take an ECG more often than younger patients.
- in patients of older age groups, MI occurs with numerous complications (pulmonary embolism - PE), stroke, pulmonary edema, pericarditis, cardiac aneurysm, complex arrhythmias and conduction disturbances), which also complicate the ECG diagnosis of MI.
PE can develop as a complication of MI, on the other hand, severe PE in elderly patients under hypoxia, hypotension and severe coronary atherosclerosis can be accompanied by myocardial infarction.
In PE, infarct-like changes are usually recorded in leads III and aVF, simulating lower diaphragmatic MI. Sometimes in V 1.2 leads, ventricular complexes such as qR, QR, Qr, QS are recorded with ST segment displacement above the isoline and T wave inversion, which gives rise to an erroneous diagnosis of anterior-posterior MI. Similar clinical signs also contribute to the misdiagnosis: chest pain, severe dyspnea, cyanosis, rhythm disturbances, and shock.
The combination of ECG changes - signs of "large-focal lower myocardial infarction", "anterior MI", acute overload of the right ventricle, tachycardia (sinus tachycardia, tachysystolic atrial fibrillation) - suggests the diagnosis of PE already on the electrocardiogram, since the anterior septal zone and the posterior wall of the myocardium are supplied from different arteries and their simultaneous blockage is extremely rare. A complete set of ECG changes in PE is rarely recorded, more often only a part of the signs are detected, and with embolism of small branches of the pulmonary artery, the ECG may remain normal.
- In addition, MI in people over 60 years of age often occurs against the background of previous ECG changes (severe ventricular hypertrophy, blockade of the branches and legs of the His bundle, WPW syndrome, cicatricial changes after myocardial infarction, ECG signs of LV aneurysm), which can cause an erroneous diagnosis (both overdiagnosis and underdiagnosis of MI).
Yes, even , contributing to the appearance of the r wave instead of the Q wave in V 1-3 leads, can hide the infarction of the septal region. Similarly, forming an r wave instead of Q waves in leads II, III, and aVF may mask signs of inferior MI.
Blockade of the posterior branch of the left NPG , increasing the amplitude of the R wave in II, III and aVF leads, can level out the signs of lower MI, translating the Q II, III, and VF teeth that are pathological in depth into non-pathological ones. In septal infarction, blockade of the posterior branch of the left IPH may mask the picture of MI by forming rS waves instead of QS.
Diagnosis of MI against the background blockade of the left NPG very difficult and often impossible on the basis of ECG data alone. Difficulties in diagnosis are caused by the following circumstances:
- Direct signs of MI and reciprocal changes in the combination of infarction and blockade of the left IPH are absent in most cases;
- the presence in leads III, aVF of the QS wave and in the right chest leads of the QS or rS wave, due to the blockade of the left NPH, on the one hand, masks the signs of myocardial infarction of the posterior and anterior septal wall of the left ventricle, and on the other hand leads to its overdiagnosis;
— The diagnosis of MI secondary to left LBBB is usually made on the basis of microsymptoms, but, however, they are not pathognomonic for MI and can be observed in LBBB without concomitant infarction. A sharp rise in the ST segment in the chest leads can be without a heart attack. Positive T waves in V 5-6, I and aVL leads can be recorded with concomitant left ventricular hypertrophy. The absence of an increase or decrease in the amplitude of the R wave in leads V 1 -V 4, known as the phenomenon of "failure" of the R wave, in the region of the transition zone should also be evaluated carefully;
- the diagnosis of acute myocardial infarction is clarified during dynamic ECG monitoring (rapid ECG dynamics), however, in acute MI developing against the background of blockade of the left IPH, the ECG picture may remain stable;
- with the blockade of the left NPG, it is difficult to determine the localization, duration and scale of the lesion. Even an indisputable sign of myocardial infarction against the background of blockade of the left NPG, as a rule, does not allow us to speak about its prescription, since it can be observed both in the acute and in the cicatricial stage;
Blockade of the right NPG does not complicate the ECG diagnosis of MI (with the exception of posterior localization infarction), but interferes with the assessment of its prevalence and depth, because with this combination, QR complexes are usually recorded, and not QS, even if the infarction is transmural.
In older age groups, the incidence repeated MI is 45%. ECG diagnosis of repeated MI against the background of cicatricial ECG changes after a heart attack is very difficult. Quite often the primary or repeated heart attack is not recognized. Repeated MI with localization in the anterior wall erases or significantly reduces the ECG signs of the first MI with localization in the posterior wall, which makes it impossible or significantly complicates its retrospective diagnosis. Posterior wall myocardial infarction does not change or slightly changes the ECG signs of a previously transferred anterior wall MI. Special localizations of some old and recent MIs that are not reflected on the ECG, the presence of intraventricular conduction disturbances, and the absence of previous electrocardiograms significantly complicate the ECG diagnosis of repeated MIs. Revealing MI in many cases is possible only when compared with anamnestic ECG, which, unfortunately, is not always possible if patients are not accustomed to save the results of a previous ECG study;
In the cicatricial stage of MI, there are difficulties in interpreting ECG changes. The erroneous diagnosis of postinfarction cardiosclerosis is most often associated with an incorrect interpretation of the Q wave (especially in lead III), the absence of an increase in the amplitude of the r wave in the right chest leads, negative T waves.
Normally, the width of the Q wave should not exceed 0.03 s, the amplitude of the Q wave in standard leads does not exceed 1/4, and in the left chest leads - 1/6 of the amplitude of the R wave following it. 1-3 is a pathology, there must be a q wave in the left chest leads. The Q wave is abnormal if it is notched or split. It is usually associated with a reduction in the height of the R wave that follows it, with the R wave often serrated or split. An abnormal Q wave is usually recorded in several leads at the same time, often combined with a negative T wave.
A pronounced Q III wave is often observed in healthy people, as well as in some diseases, for example, a pathological Q wave in lead III and less often in lead aVF can be recorded when chronic diseases lungs, usually in the presence of chronic cor pulmonale.
Wave Q III, characteristic of myocardial infarction, is necessarily combined with a pathological wave Q and VF, the width of which, even in the cicatricial stage of a heart attack, should exceed 0.02 s. ECG in lead aVF has highest value for a diagnosis. The pathological Q III wave is necessarily combined with a pronounced Q II wave (it must exceed 10% R II, especially in the acute stage).
The behavior of the Q wave during deep inspiration does not significantly affect the diagnosis: the “positional” Q wave III during deep inspiration may persist, and the Q wave indicating infarction may sometimes disappear.
Weak increase in the amplitude of the tooth r from lead V 1 to lead V 3 can be in many conditions (in elderly and senile patients - a variant of the norm, in the presence of pleuropericardial adhesions, in COPD, especially in pulmonary emphysema, with hypertrophic cardiomyopathy, with left ventricular hypertrophy, with blockade of the anterior branch of the left INH, with blockade of the left INH , with incorrect placement of chest electrodes). With MI in the anterior septal region, it matters only if there is a history of MI in this area.
As practice shows, almost the largest number of diagnostic errors in electrocardiography is made when trying to make a diagnosis, based only on the presence of negative T waves on the ECG. Considering the extreme non-specificity of this symptom, a correct diagnostic conclusion is possible only with mandatory registration clinical picture diseases, analysis of previous electrocardiograms and repeated ECG registrations.
Overdiagnosis of MI by ECG (both in the acute and in the cicatricial stage) is due to a number of reasons, among which a significant place is occupied by infarct-like ECG changes and infarct-like diseases, in which the clinical picture and ECG changes resemble MI. Moreover, false-negative ECG results are less common than false-positive ones, i.e. according to the ECG, myocardial infarction is less often missed than it is put where it is not.
The list of diseases and syndromes in which the electrocardiogram “simulates” MI (pathological Q wave, changes in the T wave and ST segment) is very extensive. It includes: myocarditis, cardiomyopathy, PE, pneumothorax, lung diseases, neuromuscular diseases - progressive muscular dystrophy, atrophic myotonia), cerebrovascular accident, acute pancreatitis, acute cholecystitis, metabolic and electrolyte disorders, ventricular hypertrophy, blockade of the branches and legs of the His bundle , WPW syndrome, early ventricular repolarization syndrome (ERVR) and others. Replacement of the heart muscle with tumor, fibrous tissue and amyloid, sarcoidosis, or other granulomas can cause the appearance of Q waves, simulating myocardial infarction. A transient pathological Q wave may appear with metabolic disorders that accompany shock of various etiologies, with uremia, hyperkalemia, Prinzmetal's angina attacks, conducting a test with physical activity, myocarditis, acute pancreatitis, acute disorders of cerebral circulation.
A number of diseases and the clinical picture resemble MI (acute pancreatitis, dissecting aortic aneurysm, pericarditis, pulmonary embolism, and others).
The correct interpretation of ECG changes is based on taking into account all available ECG signs and especially on knowledge of the clinical diagnosis. In doubtful cases, to clarify the diagnosis, it is necessary to use additional ECG leads and, of course, ECG monitoring over time.
So, when registering QS complexes in leads III and aVF with LVH and blockade of the left NPG in lead II, the Q wave is absent and QS-type complexes are not recorded, the ST segment in leads III and aVF is elevated above the isoline and merges with a positive T wave. In chest leads signs of LVH or blockade of the left NPG are recorded.
To clarify the genesis of the QS type complex in V 1-3 leads, it is recommended to take an ECG in leads V 3 R and V 4 R. If in these leads appears complex type rS, then the presence of QS in V 1-3 leads speaks in favor of focal cicatricial changes in the septal zone. With LVH and blockade of the left IPH, QS-type complexes persist.
With blockade of the anterior branch of the left NPG in the right chest leads, complexes of the QS or qrS type can be recorded, or a slight increase in the amplitude of the r wave from V 1 to V 3 leads is observed. In the chest leads, taken two intercostal spaces below the standard points, a normal increase in the amplitude of the R wave from V 1 to V 3 leads is recorded. The Q wave due to myocardial infarction persists. In addition, with blockade of the anterior branch of the left NPG, there is a sharp turn of the eos to the left and often pronounced S waves in the left chest leads.
When the chest leads of the ECG are taken two intercostal spaces below the usual level, a patient with chronic lung disease will experience a normal increase in the amplitude of the R wave from lead V 1 to lead V 4, if the QS waves or a slight increase in the amplitude of the r wave in the right chest leads were simply due to a displacement of the heart down due to emphysema.
It should be a rule:
- in the presence of pain in the left half of the chest, as well as in the places of irradiation of pain with typical angina pectoris and myocardial infarction in the elderly, it is necessary to record an ECG. Re-registration of the ECG after the end of an anginal attack is required.
- Against the background of old cicatricial ECG changes, a suddenly developed acute overload of one of the ventricles should be suspicious of repeated MI. Dynamic (including electrocardiographic) observation of the patient is necessary;
If you suspect a myocardial infarction, you must remember:
- A “normal” ECG during or immediately after a pain attack does not exclude the diagnosis of MI. After each severe and prolonged angina attack within a week, the patient should be considered suspicious for acute MI. Repeated ECG registrations are mandatory (preferably daily);
- if MI is suspected, the patient should be sent for an ECG study as soon as possible, since signs of small-focal MI may disappear with late ECG registration;
- when interpreting the Q wave, it should be taken into account: with MI in early excited areas (septum, anterior wall), the Q wave can be pathological even with a duration of 0.02-0.03 s, therefore, any Q wave located in the chest leads to the right of the transition zone is considered to be such . With MI in late excited areas (posterior, lateral wall), the Q wave will be pathological only with a duration of 0.04 s or more, or with a duration of 0.03 s, but an amplitude of more than 1/3 of the R wave. Abnormal Q wave is absent in subendocardial or intramural MI; with transmural necrosis in late excited (after 0.03-0.04 s) areas (side wall), the pathological Q wave may also be absent, and the loss of the potential of the damaged area leads to a decrease in the amplitude of the R wave and the formation or increase in the amplitude of the S wave;
- ECG changes during an angina attack in the elderly can be associated with angina pectoris only after re-registration of the ECG, when the attack was stopped, and the electrocardiogram returned to the original;
- in cases where there are no changes in the usual leads after a prolonged anginal attack, it is necessary to remove the extreme right chest leads, V 7-9 leads, leads across the Sky, chest leads two intercostal spaces above and below the standard ECG recording points;
- if a repeated MI is suspected, one should always compare it with the ECG taken earlier, conduct an ECG observation in dynamics, since in some cases it is possible to identify a repeated MI only by comparing with the ECG recorded in dynamics. At the same time, any newly appeared changes against the background of signs of myocardial fibrosis, including “positive” ones, with the existing clinic, should be interpreted in favor of myocardial infarction;
- when diagnosing MI against the background of left NIH blockade, the following tactics should be followed: the very occurrence of left NIH blockade (if it is not associated with other diseases and did not occur due to a documented gradual deterioration in intraventricular conduction) should be considered as possible sign myocardial infarction. Even the slightest change ECG patterns of the left leg block in dynamics in the appropriate clinic may indicate fresh focal changes in the myocardium, however, the absence of ECG changes in dynamics in patients with left NPG block and with suspected MI does not exclude the development of myocardial infarction;
- in a number of diseases, there may be a pseudo-infarction ECG (PE, cardiomyopathy, pericarditis, severe emphysema, WPW syndrome, and others).
Diagnosis of myocardial infarction is primarily based on clinical signs, but in all cases where acute coronary insufficiency can be suspected, urgent ECG evaluation is necessary. Changes in the electrocardiogram may be the only convincing symptom of MI with relatively short-term and easily eliminated anginal pain or other atypical clinical manifestations of the disease. On the contrary, the absence of ECG signs of coronary circulation disorders after a severe and many hours of anginal attack may give reason to suspect another pathological process and continue the diagnostic search.
It is necessary to actively work with patients. Often the correct ECG conclusion can be established only by comparing with the ECG taken earlier, it is necessary to orient patients of older age groups to save the results of the examination and recommend to patients, especially in the presence of cardiac pathology, to have the data of the previous examination with them
Hypertrophy of the myocardium of the atria and ventricles is reflected on the ECG, but the role of electrocardiography in the recognition of hypertrophy is relatively small, tk. the size of the ECG waves is influenced not only by the mass of the myocardium, but also by many other factors - the position of the heart in the chest, the thickness of the chest wall, the presence or absence of myocardial fibrosis, pathological changes in the lungs, pericardium, pleural cavity, disorders of intra-atrial and intra-ventricular conduction, etc. Therefore, very often there is no correlation between ECG data and the results of clinical and anatomical studies. Sometimes, even with severe hypertrophy, the ECG picture changes little. The most difficult thing to diagnose with the help of ECG is right ventricular (RV) hypertrophy.
ECG diagnosis of hypertrophy of the heart in the elderly and senile age is especially difficult and has some features.
Atrial hypertrophy. Even in practically healthy elderly and senile people, the ECG shows broadening, flattening and deformation of the P wave, which makes it difficult to diagnose atrial hypertrophy by ECG. In addition, in old age there are pathological conditions, which cause a decrease in the voltage of the ECG teeth, including the P wave - obesity, emphysema, effusion in the pleural cavity, heart failure and others. Therefore, the absolute values of the amplitudes of the P wave in the ECG diagnosis of atrial hypertrophy in the elderly are only of relative value, the relationship of the P waves in various leads is of primary importance. In addition, high P waves that are not associated with an increase in the right atrium (pseudo P-pulmonale and pseudo P-mitrale) can be recorded.
The main reasons for the increase in the P wave include: sinus tachycardia, sympathicotonia, hypoxemia, hypokalemia, hypocalcemia, an attack of bronchial asthma, asthenic constitution.
The main causes of pseudo P-mitrale are pulmonary emphysema, "straight back" syndrome, "cobbler's chest", which is associated with a downward displacement of the heart in the chest relative to the chest electrodes. In 30% of cases, P-pulmonale is caused by left atrial enlargement.
For the diagnosis of right atrial hypertrophy in persons over 60 years of age, the appearance of an atrial right-wing chart is important - Р III > Р II > Р I (normally Р II > Р I > Р III). The amplitude of the P II-III wave may not exceed 2-2.5 mm, but the P I wave in these cases is low-amplitude (up to 0.5 mm) or smoothed, often negative, the P aVL wave is negative, the P V 1 wave becomes high pointed or a two-phase P wave V 1, V 2 is recorded with a sharp predominance of the first positive phase of the P wave. In patients with chronic obstructive pulmonary diseases, a negative P wave can be recorded in lead V 1, which, when recording the right chest leads on two intercostal spaces below the standard ECG points, becomes high positive.
In the ECG diagnosis of left atrial hypertrophy, V 1 assignment also matters (a predominantly negative P wave or a two-phase P wave is recorded with a sharp predominance of the second negative phase) and the deviation of the electric axis of the P wave to the left (P I> P II> P III).
Left ventricular hypertrophy. ECG diagnosis of left ventricular hypertrophy in the elderly and senile is difficult, there can be both false positive and false negative diagnosis. LV is not detected. In obese people or people with certain diseases (hypothyroidism, emphysema, pleurisy, etc.), on the contrary, there may be an increase in the left ventricle without identifying criteria for left ventricular hypertrophy on the electrocardiogram.
The amplitude criteria for LV hypertrophy used for younger patients do not work in elderly patients, since even in practically healthy elderly and senile individuals, the voltage of QRS complexes on the ECG decreases. In addition, in persons over 60 years of age, there are often conditions that cause a decrease in the voltage of the ventricular complex waves and can mask ECG signs of LV hypertrophy: severe chronic obstructive pulmonary disease (COPD), obesity, hypothyroidism, heart failure, pericardial or pleural effusion , large-focal previously transferred anterior myocardial infarction, heart muscle diseases, such as amyloidosis and scleroderma, and others. In this regard, lower amplitude criteria are used for ECG diagnosis of LV hypertrophy in the elderly .
Elderly patients often have concomitant intraventricular conduction disturbances that make it difficult to detect ECG signs of LV hypertrophy. So, blockade of the anterior branch of the left NPG can cause a decrease in the amplitude of the ventricular complex and change the T waves in the left chest leads (rS-type complexes and positive T waves in V 5-6 leads), thereby masking LV hypertrophy. At the same time, blockade of the anterior branch of the left IPH can, by increasing the QRS amplitude in the limb leads, mimic LV hypertrophy. With left NPG blockade and right NPG blockade, ECG diagnosis of LV hypertrophy is almost impossible.
Often, with LV hypertrophy, the exclusion of coronary pathology is required, as follows:
- LV hypertrophy can be manifested by a weak increase in the r wave in leads V 1 -V 3, sometimes there is a significant rise in the ST segment and an increase in the amplitude of the positive T wave in these leads;
- ventricular QS complexes with ST segment elevation in III, aVF, V 1-2 leads, deep Q waves in V 5-6, I leads or the disappearance of the q wave in V 5-6, I leads with LV hypertrophy require the exclusion of myocardial infarction .
It must be remembered: when registering QS complexes in leads III and aVF leads with LV hypertrophy in lead II, the Q wave is absent and QS-type complexes are not recorded, the ST segment in leads III and aVF is elevated above the isoline and merges with the positive T wave. signs of LV hypertrophy.
To clarify the genesis of the QS type complex in V 1-3 leads, it is recommended to take an ECG in leads V 3 R and V 4 R. If an rS-type complex appears in these leads, then the presence of QS in V 1-3 leads speaks in favor of focal cicatricial changes in the septal zone (the r wave is due to excitation of the right ventricle). With left ventricular hypertrophy, QS-type complexes persist. In addition, there are signs of LV hypertrophy in the left chest leads.
When clarifying the genesis of deep Q waves in the left chest leads, it must be remembered: with LV hypertrophy, the Q wave of normal duration is combined with a high R wave, the ratio of Q waves in the left chest leads is as follows: Q V 4< Q V 5 < Q V 6 . При очаговых изменениях боковой стенки Q V 4 >Q V 5 > Q V 6 , Q waves are wide, serrated, accompanied by a decrease in R wave amplitude, deep S waves can be recorded.
- with severe LV hypertrophy, a decrease in the ST segment and negative T waves can be observed not only in leads V 5-6, but also from V 3 to V 6 leads. The assessment of clinical manifestations, the absence of rapid ECG dynamics characteristic of acute coronary pathology, and the presence of other ECG signs of LV hypertrophy help to establish the correct diagnosis. With LV hypertrophy, in each subsequent lead from V 3 to V 6, the depression of the ST segment increases, the depth of the negative T wave increases. Changes in the ST segment and the T wave, more pronounced in leads V 3 and V 4 than in leads V 5 , V 6 , indicate ischemia, i.e. the ratio of negative T waves in left ventricular hypertrophy -T V3<Т V4 <Т V5 <Т V6 , при инфаркте миокарда — Т V3 >T V4 > T V5 > T V6 ;
- with clear ECG criteria for LV hypertrophy, a decrease in the ST segment and negative T waves in leads V 1, V 2, positive T waves in V 5, V 6 leads may be due to concomitant right ventricular hypertrophy;
- with a combination of blockade of the left leg of the His bundle and LV hypertrophy in leads V 5-6, as well as in I and aVL, a positive T wave can be recorded.
ECG signs of LV hypertrophy in elderly patients
For the diagnosis of LV hypertrophy in people over 60 years of age, the following ECG criteria are recommended:
- deviation of eos to the left;
- shift of the transition zone to the right chest leads, a sharp transition from a QRS complex with a deep S wave in the chest lead to a QRS complex with a high R in the next lead located to the left, or a low-amplitude transitional lead with a shift of the transition zone to the left.
— R aVL > 7 mm;
— R V 5.6 > 16 mm;
— S V1 + R V5 or R V6 > 28 mm;
- R-wave ratio in the left chest leads - R V 6 > R V 5 > R V 4 ;
- asymmetric depression of the ST segment more than 0.5 mm and negative T waves in leads V 5 and V 6;
- indirect signs (enlargement of the left atrium, atrial fibrillation, a slight increase in the amplitude of the r waves from V 1 to V 3 leads).
Under conditions of a decrease in the voltage of the teeth of the ventricular complex in elderly and senile patients, the main, and sometimes the only reference point for the diagnosis of LV hypertrophy, often becomes the characteristic defiguration of the ST segment and the T wave and the ratio of the R waves in the left chest leads.
Right ventricular hypertrophy
Right ventricular hypertrophy in older age groups is diagnosed by electrocardiography very rarely.
The most common causes of acquired right ventricular hypertrophy are pulmonary hypertension and, more commonly, chronic obstructive pulmonary disease. With emphysema, the amplitudes of the QRS complex teeth decrease and the ECG may be normal even in the presence of severe right ventricular hypertrophy.
In chronic lung diseases and the development of S-type RV hypertrophy in V 1, V 3 leads, ventricular complexes of the QS type can be recorded, or a slight increase in the amplitude of the r wave from V 1 to V 3 leads is observed, which is explained by a significant change in the position of the heart in the chest from - for an increase in the right heart, emphysema and low standing of the diaphragm. In these cases, it is recommended to additionally record the ECG in leads V 1-6 with the position of the chest electrodes 2 ribs below the usual level. If a ventricular QS complex or a weak increase in the amplitude of the r wave in V 1 through V 3 leads is associated with a low standing diaphragm, and not myocardial infarction, then R waves increasing in magnitude from V 1 to V 3 appear in additional leads. In addition, for S-type hypertrophy of the pancreas is characterized by an electrical axis of the type S I S II S III or a deviation of the electrical axis of the heart to the right, deep S waves in the left chest leads. The anamnesis and physical data of a chronic pulmonary patient help in the diagnosis.
Chronic cor pulmonale may also resemble myocardial infarction of the lower wall of the left ventricle, since pathological Q waves can be recorded in leads III and aVF.
ECG signs of RV hypertrophy in elderly patients
The most valuable ECG criteria for right ventricular enlargement are:
- deviation of eos to the right > + 100 o;
— ratio R/S in V 1 > 1, ratio R/S in V 6< 1.
Blockade of the legs of the bundle of His and its branches, WPW syndrome, myocardial infarction, LVH make the ECG diagnosis of right ventricular hypertrophy almost impossible.
Thus, electrocardiography plays an auxiliary role in the diagnosis of cardiac chamber hypertrophy, and its results should be interpreted only taking into account the clinical picture of the disease and data from other research methods, primarily echocardiography.
A doctor of functional diagnostics working with elderly and senile patients should know the age-related features of the electrocardiogram, the age structure of morbidity, be aware of the possibility of an atypical course of diseases, take into account the use of drugs and their effects on the electrocardiogram. It should be a rule that a detailed analysis of all the information related to the patient is mandatory. medical records- It is necessary to know the state of health of a particular patient. It must also be remembered that valuable information for establishing the correct diagnosis in elderly patients can be obtained with a competent history taking and physical examination of the patient. ECG results should be evaluated in conjunction with other research methods, taking into account the individual characteristics of the patient.
Regular ECG monitoring is required:
- patients receiving antiarrhythmic drugs;
- patients receiving potentially cardiotoxic drugs (phenothiazines, antidepressants, sympathomimetics, antihypertensives, some antibiotics, etc.);
- patients with probable electrolyte disturbances (acute and chronic kidney failure, enteritis, poisoning);
- Patients with diagnosed rhythm and conduction disorders and if they are suspected.
It should be a rule:
- in the presence of pain in the left half of the chest, in the region of the left shoulder, shoulder blade, epigastrium, as well as in places of pain irradiation in a typical myocardial infarction in the elderly, it is necessary to record an ECG. Elderly people should also be referred to the ECG for stabbing pains in the chest, pains with signs inherent in pleural lesions, pains that occur mainly at rest;
- for any type of cerebral disorders in the elderly, it is imperative to record an ECG to exclude an atypically occurring MI;
- to determine the genesis of all rhythm and conduction disorders that developed suddenly, it is necessary to carefully monitor patients, including ECG monitoring, so as not to miss MI;
- dynamic (including electrocardiographic) monitoring of the patient is necessary if acute coronary pathology is suspected.
It is necessary to actively work with patients, since in many cases the correct ECG conclusion can only be established by comparison with anamnestic ECG. It is necessary to orient patients of older age groups to preserve the results of the examination and recommend that patients, especially in the presence of cardiac pathology such as left ventricular hypertrophy or previous myocardial infarction, carry with them the data of the previous examination, and patients with a history of arrhythmias who registered these seizures.
Prokopyeva S.N., Movchan L.A., Iskhakova G.G., Rosenzveig A.K.
Kazan State Medical Academy
City Consultative and Diagnostic Polyclinic for War Veterans, Kazan
War Veterans Hospital Kazan
Literature:
1. Galkin R.A., Kotelnikov G.P., Yakovlev O.G., Zakharova N.O. elderly patient. - Samara: GP "Perspective", 1999.
2. Doshchitsin V.L. Clinical electrocardiography - M.: Medits. information agency, 1999.
3. Korkushko O.V. Clinical cardiology in geriatrics. — M.: Medicine, 1980.
4. Korkushko O.V., Chebotarev D.F., Kalinovskaya E.G. Geriatrics in therapeutic practice. - Kyiv, Health, 1993.
5. A.B. de Luna. Clinical ECG Guide. — M.: Medicine, 1993.
6. Orlov V.N. Guide to electrocardiography. - M .: "Overlay", 1998.
7. Polyakov V.P., Movshovich B.L., Savelyeva G.G. Cardiology practice, I-II volumes - Samara, 1994.
8. Practical geriatrics. Ed. G.P. Kotelnikova, O.G. Yakovlev. - Samara, 1995.
9. Practical cardiology. Ed. V.V. Gorbachev. - Mn.: Higher. School, 1997.
10. Shpektor A.V., Vasiliev E.Yu. Cardiology: keys to the diagnosis. — M.: VIDAR, 1996
Small R wave growth is a common ECG symptom that is often misinterpreted by clinicians. Although this symptom is usually associated with an anterior myocardial infarction, it can be caused by other conditions that are not associated with an infarction.
A small increase in the R wave is detected in approximately 10% of hospitalized adult patients and is the sixth most common ECG abnormality (19,734 ECGs were collected by the Metropolitan Life Insurance Company over a 5 ¼ year period). Besides, one third of patients with a previous anterior myocardial infarction may have only this ECG symptom. Thus, elucidation of specific anatomical equivalents of this electrocardiographic phenomenon is of great clinical importance.
Before analyzing the changes in the R waves, it is necessary to recall several theoretical foundations that are necessary to understand the genesis of ventricular activation in the chest leads. Ventricular depolarization usually begins in the middle of the left side of the interventricular septum, and proceeds anteriorly and from left to right. This initial vector of electrical activity appears in the right and middle chest leads (V1-V3) as a small r wave (the so-called " septal wave r").
Small R-wave gains can occur when the initial depolarization vector decreases in magnitude or is directed backward. After septal activation, left ventricular depolarization dominates the rest of the depolarization process. Although the depolarization of the right ventricle occurs simultaneously with the left, its force is negligible in the heart of a normal adult. The resulting vector will be directed from leads V1-V3, and will show up as deep S waves on the ECG.
Normal distribution of R waves in the chest leads.
In lead V1, the ventricular beats are rS-type, with a steady increase in the relative size of the R waves to the left leads and a decrease in the amplitude of the S-waves. Leads V5 and V6 tend to show a qR-type complex, with R-wave amplitude greater in V5 than in V6. due to attenuation of the signal by the lung tissue.Normal variations include: narrow QS and rSr" patterns in V1, and qRs and R patterns in V5 and V6. At some point, usually in position V3 or V4, the QRS complex begins to change from predominantly negative to predominantly positive and the R/S ratio becomes >1. This zone is known as " transition zone ". In some healthy people, the transition zone can be seen as early as V2. This is called " early transition zone ". Sometimes the transition zone can be delayed until V4-V5, this is called " late transition zone ", or " transition zone delay ".
Normal R-wave height in lead V3 is usually greater than 2 mm
. If the height of the R waves in leads V1-V4 is extremely small, it is said that there is "insufficient or small increase in the R wave."
There are various definitions of small R-wave gain in the literature, criteria such asR waves less than 2-4 mm in leads V3 or V4and/or the presence of R wave regression (RV4< RV3 или RV3 < RV2 или RV2 < RV1 или любая их комбинация).
In myocardial necrosis due to infarction, a certain amount of myocardial tissue becomes electrically inert and unable to generate normal depolarization. The depolarization of the surrounding ventricular tissues at this time increases (since they are no longer resisted), and the resulting depolarization vector reorients away from the area of necrosis (in the direction of unhindered propagation). With anterior myocardial infarction, Q waves appear in the right and middle leads (V1-V4). However, Q waves are not preserved in a significant number of patients.
In documented cases of previous anterior myocardial infarction, a small increase in the R wave is detected in 20-30% of cases . The average time for the complete disappearance of pathological Q waves is 1.5 years.
Attracts attention decrease in R wave amplitude in lead I . Up to 85% of patients with a previous anterior myocardial infarction and a small increase in the R wave have either R wave amplitude in lead I<= 4 мм , or R wave amplitude in lead V3<= 1,5 мм . The absence of these amplitude criteria makes the diagnosis of anterior myocardial infarction unlikely (with the exception of 10%-15% of cases of anterior myocardial infarction).
If there is a small increase in R waves in the chest leads, Impaired repolarization (ST-T wave changes) in leads V1-V3 will increase the likelihood of diagnosing old anterior myocardial infarction.
Other possible causes of insufficient growth of the R wave in the chest leads are:
- complete / incomplete blockade of the left leg of the bundle of His,
- blockade of the anterior branch of the left leg of the bundle of His,
- the Wolf-Parkinson-White phenomenon,
- certain types of right ventricular hypertrophy (especially those associated with COPD),
- left ventricular hypertrophy
- right ventricular hypertrophy type C.

|
| Acute anterior MI |
Another common reason for a small increase in the R wave is the incorrect location of the electrodes: too high or too low location of the chest electrodes, the location of the electrodes from the limbs to the body.
Most often, the high position of the right chest electrodes leads to insufficient growth of the R waves. When the electrodes are moved to the normal position, the normal growth of the R waves is restored, however in old anterior myocardial infarction, QS complexes will persist
.
Unfortunately, these criteria turned out to be of little use for diagnosis and give many false-negative and false-positive results.
A connection between a small increase in the R wave on the ECG and diastolic dysfunction in patients with diabetes mellitus has been revealed, so this symptom may be an early sign of LV dysfunction and DCM in diabetics.
References.
- Electrocardiographic Poor R-Wave Progression. Correlation with Postmortem Findings. Michael I. Zema, M.D., Margaret Collins, M.D.; Daniel R. Alonso, M.D.; Paul Kligfield, M.D.CHEST, 79:2, FEBRUARY, 1981
- Diagnostic value of poor R-wave progression in electrocardiograms for diabetic cardiomyopathy in type 2 diabetic patients/ CLINICAL CARDIOLOGY, 33(9):559-64 (2010)
- Poor R Wave Progression in the Precordial Leads: Clinical Implications for the Diagnosis of Myocardial Infarction NICHOLAS L. DePACE, MD, JAY COLBY, BS, A-HAMID HAKKI, MD, FACC, BRUNOMANNO, MD, LEONARD N. HOROWITZ, MD, FACC , ABDULMASSIH S. ISKANDRIAN, MD, FACC. JACC Vol. 2. No. 6 December 1983"1073-9
- Poor R-Wave Progression. J InsurMed 2005;37:58–62. Ross MacKenzie, MD
- Dr. Smith's ECG Blog. Monday, June 6, 2011
- Dr. Smith's ECG Blog. Tuesday, July 5, 2011
- http://www.learntheheart.com/ Poor R Wave Progression (PRWP) ECG
- http://clinicalparamedic.wordpress.com/ R-Wave Progression: Is it important? YOU BET!!
In each electrocardiogram, 14 signs must be analyzed (Table 22-1).
Calibration and technical data
It is necessary to make sure that the electrocardiograph is correctly calibrated and the height of the calibration signal is 10 mm (1 mV = 10 mm) as described in the section "" (in special cases, the electrocardiogram is purposefully recorded at half amplification (1 mV = 5 mm) or double amplification (1 mV = 20 mm) It is important to check for grounding (see section "") and.
Rhythm frequency
Determine the heart rate. Heart rate more than 100 per minute - less than 60 per minute -.
Heart rhythm
The rhythm of the heart is almost always referred to as one of the following varieties:
- sinus rhythm (including,);
- sinus rhythm with atrial or ventricular ectopic contractions ();
- a completely ectopic (non-sinus) rhythm (for example, AF or AFL replacing the AV rhythm);
- sinus or ectopic rhythm (for example, AF) with II-III degree or.
Sometimes alternation of rhythms is observed on the electrocardiogram, for example, spontaneous restoration of sinus rhythm in paroxysmal AF.
It is especially important not to miss the hidden. So, they can be present with AV block II-III degree, atrial tachycardia with blockade, or with blocked atrial extrasystoles. Every time at a ventricular rate of about 150 beats per minute, it is necessary to exclude AF, since flutter waves can resemble teeth R with atrial or sinus tachycardia.
P-R interval
Amplitude of the QRS complex
The growth of the R wave in the chest leads
ST segment
It is important to exclude pathological or.
T wave
teeth T usually positive in leads with a positive complex QRS. In adults, they are most often positive in leads V 3 -V 6 and II, negative in lead aVR. Prong polarity T in other leads from the limbs depends on the position of the average electrical axis of the complex QRS(normal teeth T may be negative in lead III even when the axis of the complex is vertical QRS).
U wave
Expressed are a sign of hypokalemia, drug or toxic effects of drugs (for example, amiodarone, dofetilide, quinidine, sotalol).


































































