Treatment of flat feet with a 100 guarantee. Orthopedics
Plano-valgus deformity of the feet, or in common parlance longitudinal flatfoot, is one of the most common diseases in adults. The basis of the disease is a gradual, initially reversible, decrease in the height of the longitudinal internal arch of the foot, which is detected during loads, and subsequently, in the later stages, the formation of a difficult-to-remove deformity of all parts of the foot, which persists at rest.
Plano-valgus foot deformity can be congenital, but more often develops in adulthood. Its development can be facilitated by both hereditary factors and constant significant stress on the feet, for example, with excess weight or pregnancy. It has been established that one of the main causes of longitudinal flatfoot is dysfunction of the tibialis posterior tendon. This type of flat foot is characterized by quite severe pain, fatigue of the legs when walking, as well as difficulties with choosing shoes.
In this article, we will help you understand what a flat-valgus foot is, what are the causes of the development of longitudinal flatfoot, as well as how to diagnose and treat this foot deformity.
ABOUT ANATOMY AND FOOT ARCHES
The story about the anatomy of the foot should begin with the ankle joint. The ankle joint is formed by two tibia bones of the leg and the talus bone of the foot. The bones are held together by numerous strong ligaments that provide the ankle joint with essential mobility and significant stability. The ankle joint carries out movements without which normal walking, running and jumping would be impossible.
The foot can be divided into three sections: rear, middle and front. The hindfoot is formed by the calcaneus and the talus, which together form the subtalar joint. Pathology of the subtalar joint is one of the factors in the development of flat feet.

The midfoot is made up of five bones: the navicular, cuboid and three wedges. The uniqueness of the bones of the midfoot lies in the fact that under certain conditions, under the influence of muscles, ligaments of the lower leg and foot, the joints between these bones are blocked, as a result of which a fairly rigid longitudinal arch is formed on the foot. Dysfunction of some muscles and tendons of the lower leg or changes in the anatomy of the bones of the midfoot disrupts the formation of the longitudinal arch of the foot when walking, which is the trigger for the development of flat feet.

The forefoot is formed by the metatarsal bones, as well as the phalanges of the toes.
The foot is normally able to change its stiffness during walking. This is possible thanks to its complex arched vaulted design.

As noted earlier, in the anatomy of the foot, doctors distinguish between the longitudinal and transverse arches.
The transverse arch is shaped like an arc or arc formed by the metatarsal bones. The fulcrum points when walking in this arch are on the heads of the first and fifth metatarsal bones.

The calcaneus, talus, navicular, cuneiform, and first metatarsal also form an arch or arch called the longitudinal arch. The longitudinal arch, like the transverse arch, is shaped like an arc between two points of support. The support points of the transverse arch of the foot are the calcaneal tubercle and the head of the first metatarsal bone.

Tendons, ligaments and muscles of the foot
The largest and most important anatomical formation of the foot also includes the Achilles tendon. The Achilles tendon connects the calf muscle to the heel bone. The tendon got its name in honor of the ancient Greek hero Achilles. Without this tendon, we would not be able to stand on our toes or walk without limping.

Another important anatomical structure, without which it is impossible to maintain the longitudinal arch of the foot, is the tendon of the tibialis posterior muscle. The tibialis posterior tendon attaches to the navicular bone of the foot and transmits the force of the muscle of the same name to it.
In this case, the navicular bone occupies a position in which the foot has the ability to form a rigid arch and thereby perform its spring function. Damage or degeneration of the tibialis posterior tendon is a very serious problem that inevitably leads to flattening or collapse of the longitudinal arch of the foot and the development of a flat, splayed foot.
In addition to the muscles and tendons, the ligaments around the talonavicular joint play a fundamental role in maintaining the longitudinal arch of the foot.
The talocalcaneal ligament or spring ligament in combination with the tibialis posterior tendon and plantar fascia contribute to the formation and support of the longitudinal arch of the foot during walking. Stretching and rupture of the ligamentous apparatus of the talonavicular joint and navicular-calcaneal ligament (spring ligament) leads to excessive displacement of the bones of the foot relative to each other under load, and clinically manifests itself in the form of flattening of the arch and deformation of the foot, pain in the joints of the foot and ankle, as well as in painful tension of the lower leg muscles.

The uniqueness of the foot lies in the fact that individual anatomical formations, such as bones, ligaments, tendons and muscles, work together as a single mechanism, allowing us to move freely in space without experiencing pain.
WHAT IS LONGITUDINAL FLAT FOOT, AND HOW DOES THE DISEASE DEVELOP?
Plano-valgus foot, or longitudinal flatfoot, is characterized by a decrease in the internal longitudinal arch of the foot, as well as progressive deformation and impaired movement in the hindfoot.

Flattening of the longitudinal arch and deformation of the hindfoot occurs gradually as the disease progresses. Initially, a decrease in the height of the longitudinal arch and flatness of the foot can only be seen under load, for example, when the patient is standing. As the load stops, the shape of the arches and the entire foot is restored.

Subsequently, the low flattened longitudinal arch of the foot is visually determined even without any load, for example, lying down or sitting. At this stage, a clearly visible deformation of the hindfoot occurs, expressed in progressive valgus alignment and pronation of the heel bone.

As the disease progresses, there is further deformation of the hindfoot with pronation and valgus of the calcaneus. The longitudinal arch of the foot at these stages is no longer visually determined.

The foot becomes rigid, the range of motion in it decreases significantly, and the ankle joint begins to suffer. Changes in the foot at this stage are irreversible without surgical treatment. The patient's independent movement with such foot deformities, even over short distances, is either impossible or causes severe pain.
REASONS FOR WHICH LONGITUDINAL FLAT FOOT DEVELOPES
Accessory navicular bone
The presence of an additional navicular bone of the foot (os tibiale externum) is one of the main reasons for the development of longitudinal flatfoot or plano-valgus deformity of the feet.

The accessory navicular bone forms in infancy. The reason for the formation of the accessory bone is the non-fusion of several ossification nuclei responsible for the formation of the scaphoid bone. On radiographs, two navicular bones of the foot are visualized, one of which is larger than the other in size. The presence of an extra bone in itself is not dangerous to health and does not cause any discomfort for most people.
Problems arise only when the accessory bone is large in size, or when injury occurs, the fibrous connection between the bones is disrupted, which can lead to displacement of the main scaphoid relative to the accessory bone.

Often, after an injury and rupture of the fibrous tissue connecting the scaphoid bones, there is excessive mobility between the bones when walking, which also causes pain. Clinically, the patient notes the presence of a hard, painful subcutaneous formation on the instep, along the inner edge of the foot in the projection of the navicular bone. Shoes compress the large accessory navicular bone located subcutaneously, which also causes pain and swelling.
Among other things, in the area of the accessory scaphoid bone there is a site of attachment of the tendon of the posterior tibial muscle.

When walking or moving, the tendon pulls the accessory scaphoid bone away from the main bone, which also causes pain to the patient. Since the bones are split together, the tibialis posterior tendon ceases to act on the entire foot, thereby losing its role in maintaining the longitudinal arch, which leads to a gradual flattening of the foot.
Tibialis posterior tendon dysfunction
Degenerative or traumatic damage to the posterior tibial tendon is another reason, and perhaps the most important one, leading to the development of longitudinal flatfoot or plano-valgus foot deformity.

Let us recall that the tendon of the tibialis muscle is attached to the tuberosity of the navicular bone, transmits traction to the muscle of the same name, including participating in maintaining the arch of the foot when walking.
With age or in the presence of chronic diseases, such as rheumatoid arthritis or diabetes, gradual degenerative degeneration of the tendon occurs. The tendon consists of collagen fibers that are arranged in a special way. For better understanding, a tendon can be compared to a rope consisting of many intertwined threads.

This structure and arrangement of individual threads makes it very tensile. The arrangement of collagen fibers in the tendon with age or as a result of microtrauma begins to be disrupted and replaced by scar tissue.
The result of degeneration can be a significant weakening of the tendon's strength, which sets the stage for its rupture. When the tibialis posterior tendon is ruptured or stretched, its function in maintaining the longitudinal arch is lost.
Weakness of the foot ligaments
In the development of flat feet, rupture or stretching of the ligamentous apparatus of the joints of the middle and hindfoot also plays a certain role. As a result of ligament failure, instability develops in the joints of the foot, which leads to subluxation of the bones and their constituents.
For example, subluxation of the calcaneus in the subtalar joint or displacement of the navicular bone in the talonavicular joint due to damage to the spring ligament. Foot sprains can occur in patients who are overweight, have diabetes, or have conditions that impair blood circulation in the foot.
SYMPTOMS OF FLAT FOOT
The first thing a patient with flat feet notices is pain and swelling in the foot area, usually along the medial or inner surface. Patients mainly note discomfort in the leg at the end of the day or after standing for a long time. Some patients complain that they cannot stand on their toes and fully engage in sports.

DIAGNOSTICS FLAT FOOT
Taking an anamnesis (medical history) and clinical examination of the patient are the most important tools in the doctor’s arsenal in order to diagnose flat feet. The wear patterns of your shoes can also provide important information about the condition of your feet. Next, the doctor will ask you to undergo several clinical tests, for example, asking you to stand up and stand on your toes. The doctor also examines muscle strength and the condition of tendons, ligaments of the foot and lower leg. Depending on how much the longitudinal inner arch of the foot is flattened, the doctor can judge the degree of the disease.

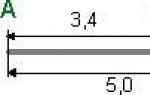
It is mandatory to perform a plantogram in the diagnosis of longitudinal flatfoot and planovalgus deformity of the feet. A plantogram is the taking of an imprint of your foot using a special device. Using the plantogram, you can determine the degree of flatfoot and thereby judge the extent of the disease.

X-rays in special projections are also used by the doctor to study the position of the bones of the foot relative to each other under load while standing or at rest while lying down.
MRI imaging is used to evaluate the condition of muscles, tendons and ligaments. For example, inflammation (tenidinitis) of the posterior tibial tendon is not visualized on an x-ray, but is clearly visible on MRI scans.

Based on radiological data, plantography and clinical picture, the doctor determines the degree of longitudinal flatfoot or plano-valgus deformation of the feet and, depending on this, prescribes a specific treatment.
With the first degrees of longitudinal flatfoot, you can do without surgery and prescribe conservative treatment. In case of severe deformities, surgery is no longer possible.
The scope of the operation is determined individually based on the degree of longitudinal flatfoot or plano-valgus deformation of the feet, age, as well as the patient’s requirements for everyday and sports activities.
CONSERVATIVE TREATMENT OF LONGITUDINAL FLAT FOOT
With initial manifestations of longitudinal flatfoot or plano-valgus deformation of the feet, conservative treatment may be recommended. In the initial stages of flat feet, the foot is still elastic, so choosing shoes with good support for the longitudinal arch of the foot can bring noticeable relief to the patient. Also, in order to correct the longitudinal arch of the foot and prevent further progression of the deformity, the manufacture of individual orthopedic insoles or arch supports may be recommended.

The orthopedic insole is made of special materials that become plastic when heated. Next, the insole is modeled individually according to the patient’s foot, and when it cools, it retains the given shape. The manufactured insole is placed inside everyday shoes. The service life of orthopedic insoles is from 6 to 12 months. Custom orthotics are probably one of the best ways to prevent flat feet.
SURGICAL TREATMENT OF LONGITUDINAL FLAT FOOT AND PLANO-VALGUS FOOT DEFORMITY
In cases where conservative treatment is not able to relieve the patient of pain and constant discomfort when moving, and the deformity of the foot increases, you can think about surgery.
There are a huge number of operations performed for longitudinal flatfoot or plano-valgus foot deformity. In our clinic we perform operations that have proven themselves over a long period of time and are widely used abroad.
Operations for flat feet 1-2 stages.
One of the main reasons for the development of longitudinal flatfoot and plano-valgus deformity of the feet is dysfunction of the posterior tibial tendon.

The unique function of the tibialis posterior muscle is that it raises the longitudinal arch of the foot in a special way and fixes this position when walking. If the function of the posterior tibial tendon is impaired for any reason, longitudinal flatfoot develops.
In the initial stages of the disease, when the foot is still elastic and the patient is young, preference is given to the most minimally invasive operations.
The most minimally traumatic operations used for longitudinal flatfoot or plano-valgus deformity of the feet and giving excellent results include subtalar arthreroeresis. The essence of the operation is to insert a special implant into the joint area between the heel and talus bones.

With longitudinal flatfoot or plano-valgus deformity, hyperpronation of the heel is observed, associated with instability and weakening of the subtalar joint ligaments. An implant inserted near the subtalar joint blocks pronation of the heel, resulting in correction of the height of the longitudinal arch.

Clinically, patients note a decrease in pain and fatigue when walking, restoration of normal gait, as well as the elimination of all restrictions in the selection and wearing of shoes.

Arthroeresis is usually combined with surgery on the tibialis posterior tendon. If tendonitis or inflammation of the tendon occurs, minimally invasive debridement is performed. The purpose of the operation is to remove thickened, inflamed and damaged tissue in the tendon area.

The operation is performed minimally invasively through small incisions using arthroscopy. After surgery, pain is significantly reduced, and the risk of degenerative rupture of the posterior tibial tendon is also reduced.
If the tibialis posterior tendon ruptures, it will need to be repaired. For ordinary ruptures, a special suture is placed on the tendon; in cases where the tendon tissue has significant pathological changes, its prosthetics (replacement) with a graft may be required.
Sometimes the posterior tibial tendon undergoes such significant degenerative changes that its restoration is futile. In such cases, the surgeon transplants a tendon from another muscle to the scaphoid bone to replace the damaged tendon of the tibialis posterior muscle.

For these purposes, the flexor of the toes is used. After the transferred digital flexor tendon grows into the navicular bone of the foot, it begins to fully work in place of the damaged tendon of the tibialis posterior muscle and instead perform the function of supporting the longitudinal arch of the foot.

The most commonly used surgical intervention in the treatment of longitudinal flatfoot, which is caused by the presence of an accessory scaphoid bone, is the operation of subtalar arthroeresis in combination with refixation of the posterior tibial tendon. In this process, the accessory bone and the inflamed, painful tissue around it are removed, and the tibialis posterior tendon, which attaches to the accessory bone, is cut off and transferred to the main scaphoid bone.

Special anchors or interference screws may be required to secure the tibialis posterior tendon. These types of fixators allow the displaced tendon to be firmly attached to the scaphoid bone until it is completely fused with it.
After surgery, patients experience restoration of the height of the arch of the foot, normalization of gait, as well as relief of pain caused by the presence of a large accessory bone in the arch of the foot.
Operations for flat feet 2-3 degrees.
In the treatment of longitudinal flatfoot or plano-valgus deformation of the feet, especially in young patients, various corrective osteotomies are also used. Osteotomy is an operation in which the bone is crossed with special instruments, the fragments are displaced and fixed in a new, more advantageous position.

The purpose of the operation is to eliminate the deformity. Osteotomies are preferred over arthrodesis, especially in young patients with minor deformities and less severely damaged joints of the foot. Arthrodesis is actually the excision of a joint followed by fusion of the bones that make it up.

Arthrodesis is a forced operation, and it is performed only when other types of operations can no longer help the patient. In orthopedics for longitudinal flatfoot and planovalgus deformity of the feet, various types of osteotomies and arthrodeses of one or more joints of the foot are used.

When choosing an operation, the surgeon takes into account many factors and individual characteristics of the patient. For example, in practice there is often a combination of longitudinal and transverse flatfoot, manifested by valgus deformity of the first toe. In such cases, surgical intervention should be aimed at eliminating all types of deformities.
Operations for flat feet 4th century.
Finally, in the case of fixed rigid longitudinal flatfoot with severe deformation, a so-called triple arthrodesis is required. Triple arthrodesis is most justified for the treatment of patients with advanced flat feet. This operation is a kind of “gold standard” in the treatment of foot deformities. This type of surgery can relieve patients from severe pain caused by arthrosis of the foot joints. With triple arthrodesis, the calcaneal-talar, talonavicular and calcaneocuboid joints are closed.

Due to the fact that during the operation, worn-out inflamed joints are excised, the patient notes a significant reduction in pain. The operation allows not only to eliminate the deformity, but also to restore and securely fix the longitudinal arch of the foot. The success of the operation for arthrodesis of the foot joints also largely depends on the quality of the fixators used. During the operation, a wide range of metal fixators (wires, staples, screws, plates) of various sizes and shapes is used.

Our clinic uses only modern high-tech foreign fixators, which reliably hold the bones of the foot in a given position until they are completely fused. All braces are specifically designed for foot surgery.

In conclusion, it is worth noting that due to the huge variety of surgical interventions used for flat feet, the final decision on the type and extent of the operation is made by the surgeon together with the patient.
The optimal result in the treatment of longitudinal flatfoot and planovalgus deformity of the feet can only be achieved through close interaction between the doctor and the patient.
WHY SHOULD YOU BE TREATED WITH US?
Our clinic uses only effective and modern methods of surgical correction of longitudinal flatfoot and planovalgus deformity of the feet.
Surgical interventions are performed using modern medical equipment from major global manufacturers.
It is also important that the result of the operation depends not only on the equipment and quality of metal fixators, but also on the skill and experience of orthopedic surgeons. The specialists of our clinic have extensive experience in treating diseases of this localization for many years.
Video about our traumatology and orthopedics clinic
PRICES FOR OUR SERVICES
Initial consultation with a traumatologist-orthopedist, Ph.D. — 1500 rubles
- Studying the patient's medical history and complaints
- Clinical examination
- Identifying symptoms of the disease
- Study and interpretation of MRI, CT and X-ray results, as well as blood tests
- Establishing a diagnosis
- Purpose of treatment
Repeated consultation with a traumatologist-orthopedist, Ph.D. - for free
- Analysis of the results of studies prescribed during the initial consultation
- Establishing diagnosis
- Purpose of treatment
Reconstruction of feet for longitudinal flatfoot 1-2 degrees. — from 39,000 to 69,000 rubles depending on the degree of deformation, volume of surgery and number of implants
- Stay at the clinic
- Anesthesia
- Operation
*
Reconstruction of feet for longitudinal flatfoot 2-3 degrees. — from 69,000 to 99,000 rubles depending on the degree of deformation, volume of surgery and number of implants
- Stay at the clinic
- Anesthesia
- Operation
- Consumables and special screws for surgery
* Tests for hospitalization are not included in the price
Reconstruction of feet for longitudinal flatfoot 3-4 degrees. — from 99,000 to 159,000 rubles depending on the degree of deformation, the volume of surgery, and the number of implants
- Stay at the clinic
- Anesthesia
- Operation
- Consumables and special screws for surgery
* Tests for hospitalization are not included in the price
Manufacturing of individual orthopedic insoles - 4900 rubles
- Clinical examination and plantoscopy
- Manufacturing of individual orthopedic insoles
- Consumables
- Recommendations for the prevention of foot diseases
Appointment with a traumatologist - orthopedist, Ph.D. after surgery - free of charge
- Clinical examination after surgery
- View and interpret the results of radiographs, MRI, CT after surgery
- Recommendations for further recovery and rehabilitation
- Dressings or removal of postoperative sutures
Contrary to the good old jokes about evading the army, flat feet are not a trivial ailment at all, but a serious orthopedic problem that can lead to many chronic diseases. Changes in the shape of the foot begin in childhood, so the sooner parents suspect something is wrong and show the child to the doctor, the better. Let's figure out where flat feet in children come from and how to deal with it.
0–3 years
At about a year old, an important event occurs in the baby’s life - the transition to a vertical position: the child takes his first steps, learning about the surrounding space. Up to 3 years of age, children’s feet are surrounded by a developed fat layer and visually have a flat surface, and the musculoskeletal system is not yet sufficiently developed. When a child begins to take his first steps, the fatty “pads” on the soles take on the function of springs. Gradually, the experience of independent active movements in space accumulates, and the foot takes on a normal appearance.
During this period, three pressure points form on the baby's foot, located on the heel, the area near the little toe and in the area under the big toe. These sections are fastened together by ligaments, muscles and tendons, so the entire structure forms three arches - two longitudinal (external and internal) and transverse. When walking, they act as shock absorbers, thanks to them the gait becomes light, and the legs get used to long hours of stress.
Now imagine that the arches of the foot - a kind of arches that pass between every two pressure points - sometimes, due to improper development of the musculoskeletal system (as well as some diseases), turn into straight lines and become flattened. It is no coincidence that when translated from English, flat feet are literally translated as “fallen arch.”
However, young children are not diagnosed with flat feet. However, if the child began to walk very early (before 9 months), suffered from rickets or has a hereditary predisposition to flat feet, the orthopedist can prescribe a prevention program that includes massage of the lower extremities, walking on an orthopedic rug and wearing orthopedic preventive shoes.
The purpose of such shoes is to develop the correct walking skill: the brain “remembers” the sequence of contraction and relaxation of muscles to perform a step, thanks to which the child continues to walk correctly even barefoot.
3–7 years
At this age, children develop the “adult” shape of the arches of the feet, and it is at this time that the orthopedist most often detects signs of pathology. Additional causes of flat feet in children of kindergarten age are excess weight, neurological and endocrine diseases. The disease can be suspected if the child places his legs oddly when walking, and after a long walk begins to limp.
The treatment and preventive program prescribed by the orthopedist involves the child performing special gymnastic exercises every day, swimming with fins, and sometimes physical therapy to improve muscle tone. In recent years, the technique of functional taping has become especially popular - gluing special adhesive tapes onto the patient’s body to tighten the skin and ease the load on joints and muscles. The prognosis for treatment among children of this age is favorable.
Simple rules of prevention will help prevent the development of flat feet in preschool children:
- Buy your child comfortable shoes that fit tightly;
- the height of the heel should not exceed 3 cm;
- allow your child to walk barefoot on uneven surfaces - bare ground, grass, sand;
- if possible, build a special path in the yard or at the dacha from wooden boards with many sections filled with various materials - gravel, cones, sand, etc.;
- the child’s diet should contain sufficient quantities of foods rich in calcium, phosphorus and vitamin D (they are important for the normal development of the musculoskeletal system);
- Make sure your child gets physical activity every day.
After 7 years
In first-graders, the arches of the feet have almost completed their development. With flat feet at this age, the first complications may appear in the form of pain in the legs and poor posture. This occurs due to the loss of the shock-absorbing function of the foot: all shocks during running and walking are transmitted to the upper joints and spine, damaging them. Over time, this can lead to arthrosis of the joints and early osteochondrosis of the spine.

How can you help a child with flat feet? Choose the right sports section for him with limited running and jumping exercises, buy orthopedic insoles (they will help avoid complications), and regularly enroll in courses of physical procedures indicated for this disease. Such measures will help prevent further deformation of the foot bones, rapid fatigue when walking and running, and poor posture.
Speaking about flat feet in children, I want to note two important aspects. Firstly, many parents do not take the disease seriously enough, and secondly, there is an overdiagnosis of this pathology among specialists. The first leads to a delayed start of treatment (let me remind you that the best results are observed when diagnosed at 3–7 years). The second is the pointless treatment of healthy feet.
It is extremely important to find an orthopedic doctor whom you are willing to trust and see your child with him at least once a year before starting school. This will help you find out about the problem in time and keep children's legs strong and healthy!
Nikolay Nigamadyanov
Photo istockphoto.com
Among the very first signs of flat feet are the occurrence of discomfort when wearing shoes and the development of an incorrect gait. There will be almost no doubt if you carefully examine the footprint left on the floor - it can clearly indicate an existing pathology.
So, it’s worth considering in as much detail as possible what it is and for what reasons it can arise.
The concept of flat feet includes various changes or deformations of the arches of the feet, as a result of which a person loses the ability to absorb shock.
It is worth mentioning that a healthy normal foot has three arches - a transverse and two longitudinal.
Like all diseases, the appearance and further development of flat feet can be prevented, so it is worth paying close attention to this issue.
The age of the patient also plays an important role, since children are more prone to this disease. This is due to the fact that until about the age of seven, the foot has not yet fully formed, so it is prone to various negative external factors.
They ultimately lead to the appearance of the disease.

It is important to note that among the types of flatfoot there are longitudinal, transverse and combined. For prevention, it is important for all people to learn how to properly distribute the load, which in the future will not only help strengthen muscles, but also improve their overall health.
Treatment and prevention of flat feet
In order for the feet to function correctly, the load must be distributed evenly across all ligaments and muscles. This is the only way to avoid any problems with your legs. If the ligaments and muscles become weaker, the feet begin to undergo deformation, and various defects arise. As a result, the foot becomes straighter and sags over time.
Among the most unpleasant aspects, it should be noted the loss of shock absorption ability, while the height of the arches gradually decreases. In IT
This often leads to a feeling of extreme fatigue, pain and discomfort in the legs, especially when walking for a long time.
After some time, the feet become thicker and larger in size. Because of this, various painful sensations in the legs, swelling and a feeling as if the foot is burning can occur.
If you experience at least one of these signs, you should immediately consult a doctor to take the necessary measures.
There are the following types of flat feet:
This disease can be divided into various types. The rarest type is considered to be a congenital type of flatfoot, which appears due to disruptions in intrauterine development.
The most common type of flatfoot is considered acquired - one that appears as a result of exposure to external factors. Acquired flat feet include the following:
- Rachitic, which arose as a result of rickets;
- Traumatic, resulting from fractures or injuries;
- Paralytic. It can occur as a result of polio, since in this case paralysis of the tibial muscles occurs.
If longitudinal flatfoot occurs, the muscles of the lower leg and foot, as well as the ligamentous apparatus of the bones, weaken. All this leads to the lowering of the longitudinal arch of the foot, and the heel turns out due to the displacement of the tendons.
In the very early stages of the disease, it all comes down to weakening of the ligaments, this is especially felt when walking, but as soon as you get proper rest, everything goes away very quickly.
There are the following degrees of flat feet.
The longitudinal has three degrees, and the transverse has four. This disease progresses gradually. There are several stages of this disease:
- Prodromal, during which the disease only begins to manifest itself as constant fatigue and pain in the legs. During this period, you need to start fighting it in order to prevent further development of the disease. In this case, gymnastics, massage, constant muscle training, and developing the correct gait will be useful.
- Intermittent. During this period, the pain is felt much more strongly, especially in those women who like to wear high-heeled shoes. During this period, the foot is most susceptible to losing its arch and may become flat. Usually this condition goes away after sleep.
In order to understand the degree of the disease, it is necessary to undergo digital podometry or radiography.
However, if the foot does not begin to function normally even after sleep, the time comes for the next stage, which is accompanied by the development of a flat foot.
The pain does not stop, and the person may experience it constantly. The gait and shape of the foot also changes significantly.
At this stage, flat feet are divided into different degrees, at which a flat foot can be formed, the arch of which will be 35 mm in height. In addition, the appearance of splayed foot or osteoarthritis is possible.

Planovalgus foot deformity
If treatment is ignored, hallux valgus may occur, which is characterized, in addition to constant pain in the limbs, by thickening of the foot and inversion.
Such a deformity is called valgus. It is important to note that at such an advanced stage it is no longer possible to solve the problem using therapeutic methods.
There is only one option left, namely surgery, which should be planned according to the condition and characteristics of the disease of each individual patient.

Those who spend most of their time on their feet, as well as overweight patients, are more susceptible to this disease.
Among women, the most common cause may be frequent wearing of low-quality high-heeled shoes.
The best shoes will be models made of soft leather with flexible soles and low, maximum 5 centimeters, heels.
The toe box should be wide, but you should not wear shoes that are too wide and loose, as this leads to chafing, calluses and inflammation.
However, tight shoes are also harmful, because in addition to calluses, they lead to ingrown nails, bent fingers and impaired blood supply. It is best if the shoes fit the foot like a second skin.
To keep your feet healthy for as long as possible, you should practice self-massage of your feet, take foot baths, and wear only high-quality, comfortable shoes with custom orthopedic insoles.
Such shoes can successfully take over some functions, thereby relieving problem areas of the feet.
In more advanced cases, it is necessary to choose orthopedic shoes that will help prevent the occurrence of various foot deformities and correct them if they have already occurred.
With this disease there is foot deformity, which looks like this: the arch of the foot decreases, the foot itself becomes flatter, and in severe cases it almost completely flattens. Flat feet can develop over quite a long time, and in the initial stages a person, as a rule, does not understand what is happening to him and where the unpleasant sensations come from. Let's try to figure it out where does flat feet come from, what are the negative factors, contributing to its development, into what degrees it is divided and how to treat this condition.
In a normal state, the human foot has two arches: in the direction from the heel to the toes there is a longitudinal arch, and in the forefoot, under the bases of the toes, there is a transverse arch. Both arches are necessary for confidently maintaining balance and protect against shaking when walking, that is, they work as natural shock absorbers. With flat feet, this important shock-absorbing function begins to decrease, as a result of which the load on higher joints and the spine increases, and various complications arise.
Causes and risk factors for flat feet
 Play a decisive role in the development of this disease heredity and physical inactivity, that is, a sedentary lifestyle. Under the influence of these and other unfavorable circumstances, the muscles and ligaments that support the foot weaken, the foot becomes deformed and begins to lose shock absorption capabilities. Depending on which of the arches of the foot changes pathologically (lowers), transverse and longitudinal flat feet are distinguished. Combined flatfoot, that is, a combination of the two types mentioned, is often diagnosed.
Play a decisive role in the development of this disease heredity and physical inactivity, that is, a sedentary lifestyle. Under the influence of these and other unfavorable circumstances, the muscles and ligaments that support the foot weaken, the foot becomes deformed and begins to lose shock absorption capabilities. Depending on which of the arches of the foot changes pathologically (lowers), transverse and longitudinal flat feet are distinguished. Combined flatfoot, that is, a combination of the two types mentioned, is often diagnosed.
 Note that transverse flatfoot– this is a problem exclusively for adults; it does not happen to children. A number of babies are born with a flat-valgus foot, and this is a physiologically normal phenomenon, but often there is a flat-valgus foot placement, which is much more pronounced than the physiological norm. In such cases, it is important not to let the situation get worse, to be observed by an orthopedist and to correct this pathology from an early age, as soon as the child begins to walk (around one and a half years). Therapy usually involves wearing orthotics, performing special exercises and therapeutic massage sessions. The diagnosis of “flat feet” can only be made after reaching seven years of age. Timely treatment, even in childhood, will allow you to avoid gait disturbances and the most unfavorable consequences of flat feet: increased load on higher joints, the occurrence of early arthrosis.
Note that transverse flatfoot– this is a problem exclusively for adults; it does not happen to children. A number of babies are born with a flat-valgus foot, and this is a physiologically normal phenomenon, but often there is a flat-valgus foot placement, which is much more pronounced than the physiological norm. In such cases, it is important not to let the situation get worse, to be observed by an orthopedist and to correct this pathology from an early age, as soon as the child begins to walk (around one and a half years). Therapy usually involves wearing orthotics, performing special exercises and therapeutic massage sessions. The diagnosis of “flat feet” can only be made after reaching seven years of age. Timely treatment, even in childhood, will allow you to avoid gait disturbances and the most unfavorable consequences of flat feet: increased load on higher joints, the occurrence of early arthrosis.
In addition to heredity and a significant lack of movement, the following reasons can affect the development of flat feet:
- being overweight;
- frequent wearing of excessively narrow and uncomfortable shoes, high heels;
- consequences of previous injuries: sprains, fractures, injuries to the soft tissues of the foot;
- presence of osteoporosis, previous rickets;
- paralysis of the foot muscles;
- excessively intense and prolonged stress on the legs (sports training, heavy physical labor, prolonged standing, stress associated with pregnancy, etc.).
Signs and degrees of flat feet
Whatever worries you, do not engage in self-diagnosis and self-medication - this will not bring the necessary positive result and may even be dangerous. If you suspect that you may have flat feet, consult with a podiatrist who, after examination and examination, will diagnose a foot deformity or, if another pathology is discovered, will refer you to a specialist in a different field (some signs inherent in flat feet may also be symptoms of varicose veins or other diseases). By what signs can you suspect that you are developing flat feet?
- fatigue in the legs when walking, pain in the feet after standing for a long time or other physical activity;
- swelling, a feeling of heaviness, possible cramps in the calves;
- footwear trampling on one side;
- pain in the knees, hip joints, lower back;
- the need to purchase larger shoes than before.
 For longitudinal flat feet Painful sensations in the feet are constant, the feet swell, and pressure on them can in some cases cause pain. Pain can also be felt in the legs, and the spine suffers. Transverse flatfoot is characterized by such signs as deformation of the forefoot and toes, pain in the forefoot, and you may notice the appearance of calluses and experience problems with selecting and wearing shoes.
For longitudinal flat feet Painful sensations in the feet are constant, the feet swell, and pressure on them can in some cases cause pain. Pain can also be felt in the legs, and the spine suffers. Transverse flatfoot is characterized by such signs as deformation of the forefoot and toes, pain in the forefoot, and you may notice the appearance of calluses and experience problems with selecting and wearing shoes.
There are three degrees in the development of longitudinal flatfoot. In the first degree, the shape of the foot is slightly changed, but the person’s legs ache after exercise and may swell, but by morning they return to normal. In the second degree, the foot changes its configuration more strongly, becomes more flattened, and the arches begin to smooth out. The pain is intense, covers the ankle and spreads to the higher joints - the knee and hip; with prolonged walking, fatigue and pain occur. In the third degree, the foot is already significantly deformed, walking in ordinary shoes is completely impossible, due to constant pain, the person becomes unable to work and is inactive, and the quality of life suffers.
How and why to treat flat feet?
If you notice any alarming signs, do not wait for pathological changes in the foot, get diagnosed and treated. Timely and competently carried out conservative treatment will protect you from increased stress on the ankle, knee, hip joints and spine, and, accordingly, from the development of complications such as arthrosis, osteochondrosis, scoliosis and other diseases. And, of course, the treatment will provide relief from pain, discomfort when walking and will return a good quality of life and the ability to move freely.
 All types of flat feet are corrected primarily by wearing custom-made orthopedic insoles. The insoles model the arches of the foot, evenly distribute the load, and have a shock-absorbing function. Do not buy insoles yourself: an orthopedist should select them for you, taking into account all the features of your foot. In addition, it is necessary to strengthen the muscles of the foot - do a set of special exercises and general strengthening gymnastics daily. It is recommended to walk barefoot on various natural surfaces - sand, pebbles, grass, but it is extremely undesirable to walk on artificial ones, for example, parquet or carpet. Swimming and cycling are very useful and give preference to those sports where there are no static loads. A comprehensive treatment program usually also includes physiotherapy procedures, massage, drug therapy for pain relief, various measures to help relieve tension in the legs. As a result of treatment, the muscular-ligamentous apparatus is strengthened, the arches of the feet are corrected and the disease stops progressing.
All types of flat feet are corrected primarily by wearing custom-made orthopedic insoles. The insoles model the arches of the foot, evenly distribute the load, and have a shock-absorbing function. Do not buy insoles yourself: an orthopedist should select them for you, taking into account all the features of your foot. In addition, it is necessary to strengthen the muscles of the foot - do a set of special exercises and general strengthening gymnastics daily. It is recommended to walk barefoot on various natural surfaces - sand, pebbles, grass, but it is extremely undesirable to walk on artificial ones, for example, parquet or carpet. Swimming and cycling are very useful and give preference to those sports where there are no static loads. A comprehensive treatment program usually also includes physiotherapy procedures, massage, drug therapy for pain relief, various measures to help relieve tension in the legs. As a result of treatment, the muscular-ligamentous apparatus is strengthened, the arches of the feet are corrected and the disease stops progressing.
If transverse flatfoot is diagnosed in the initial stage, it is necessary to take measures to correct it in order to prevent the increase in deformity, which often occurs quite rapidly. In situations where severe deformity of the forefoot is observed, when conservative therapy is ineffective, to improve the quality of life and return the patient to the ability to move normally, a decision may be made to undergo surgery. Its technique and volume are determined individually by the surgeon.
Contact an orthopedic specialist if you have any suspicious symptoms in the area of the feet and lower extremities, because flat feet are a serious condition and its correction should be dealt with only with the qualified help of an experienced doctor.
Make an appointment with an orthopedist
Be sure to consult a qualified specialist in the field of orthopedic diseases at the Semeynaya clinic.